
Thrombocytopoiesis process, stimulants, regulation

The thrombocytopoiesis It is the process of formation and release of platelets. This process takes place in the bone marrow just like erythropoiesis and granulopoiesis. Platelet formation comprises two phases: megakaryopoiesis and thrombocytopoiesis. Megakaryopoiesis begins from the precursor cell of the myeloid lineage until the formation of the mature megakaryocyte.
On the other hand, thrombocytopoiesis comprises a series of events through which the megakaryocyte passes. This cell receives different signals depending on where it is..
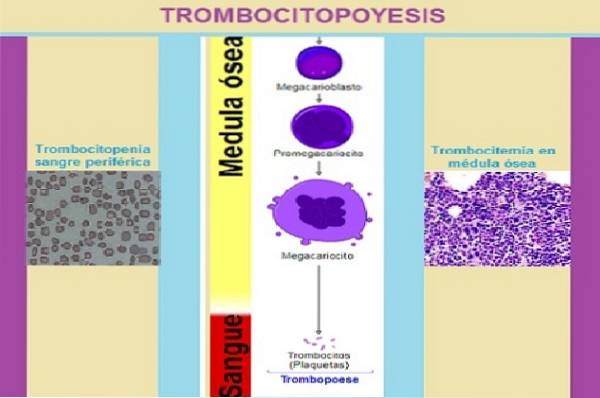
As long as the cell is within the osteoblastic stroma, it will be inhibited, but when it leaves the extracellular space of the vascular compartment, it is activated by the presence of stimulating substances..
These substances are von Willebrand factor, fibrinogen, and vascular endothelial growth factor. Once activated, the cytoplasmic processes of the megakaryocyte called proplatelets will fragment to give rise to the proplatelets and platelets..
Thanks to the process of regulation of thrombocytopoiesis, it is possible to maintain homeostasis in terms of the circulating number of platelets. As thrombocytopoiesis stimulating factors there are thrombopoietin, interleukin 3 (IL3), IL 6, and IL 11. And as inhibitory factors are platelet factor 4 and transforming growth factor (TGF) β.
There are various diseases in which the number of circulating platelets is altered, as well as their morphology or function. These abnormalities create serious problems in the individual who suffers them, especially bleeding and thrombosis, among other complications..
Article index
- 1 Process of thrombocytopoiesis
- 1.1 -Megakaryocytopoiesis
- 1.2 -Thrombocytopoiesis
- 2 Stimulants of thrombocytopoiesis
- 2.1 Interleukin 3
- 2.2 Interleukin 6
- 2.3 Interlequin 11
- 2.4 Thrombopoietin
- 3 Regulation of thrombocytopoiesis
- 3.1 -Thrombopoietin
- 3.2 -Inhibitory factors
- 4 Diseases produced by imbalance in thrombocytopoiesis
- 4.1 Congenital amegakaryocytic thrombocytopenia
- 4.2 Essential thrombocythemia
- 4.3 Thrombocytopenia
- 4.4 Bernard-Soulier syndrome
- 4.5 Immune thrombocytopenic purpura
- 5 References
Thrombocytopoiesis process
Platelet formation can be divided into two processes, the first is called megakaryocytopoiesis and the second is thrombocytopoiesis..
As is known, all cell lines come from the pluripotential stem cell. This cell differentiates into two types of progenitor cells, one from the myeloid lineage and the other from the lymphoid lineage..
2 types of cells arise from the progenitor cell of the myeloid lineage, a megakaryocytic-erythroid progenitor and a granulocytic-macrophage progenitor.
Megakaryocytes and erythrocytes are formed from the megakaryocytic-erythroid progenitor cell.
-Megakaryocytopoiesis
Megakaryocytopoiesis comprises the process of differentiation and maturation of cells from the burst-forming unit (BFU-Meg) until the formation of the megakaryocyte.
CUF-GEMM
This cell arises from the stem cell and from it the progenitor cells of the granulocytic-macrophage and megakaryocytic-erythroid cell lines are derived..
BFU-Meg
This cell is the earliest specimen of the megakaryocytic series. It has great proliferative capacity. It is characterized by presenting the CD34 + / HLADR receptor on its membrane-
CFU-Meg
Its proliferative capacity is less than the previous one. It is a little more differentiated than the previous one and in its membrane it presents the CD34 + / HLADR receptor+
Promegacarioblast
Measuring 25 and 50 µm, it has a large, irregularly shaped nucleus. The cytoplasm is slightly basophilic and may have slight polychromasia. It can have from 0 to 2 nucleoli.
Megakaryoblast
This cell is characterized by being smaller in size than the megakaryocyte (15-30 µm), but much larger than other cells. It usually has a visible bilobed nucleus, although it can sometimes exist without lobulations.
The chromatin is lax and several nucleoli can be appreciated. The cytoplasm is basophilic and scant.
Promegacariocito
This cell is characterized by having a polylobulated and notched nucleus. The cytoplasm is more abundant and is distinguished by being polychromatic.
Megakaryocyte
This is the largest cell, measuring between 40-60 µm, although megakaryocytes measuring 100 µm have been seen. Megakaryocytes have abundant cytoplasm, which is usually eosinophilic. Its nucleus is polyploid, large and has several lobulations.
In the maturation process of this cell, it acquires characteristics of the lineage, such as the appearance of specific platelet granules (azurophils), or the synthesis of certain components of the cytoskeleton such as actin, tubulin, filamin, alpha-1 actinin and myosin..
They also present invagination of the cell membrane that forms a complex membrane demarcation system that will extend throughout the cytoplasm. The latter is very important because it is the basis for the formation of platelet membranes..
Other characteristics of these cells are the following:
- Appearance of specific markers in its membrane, such as: glycoprotein IIbIIIa, CD 41 and CD 61 (fibrinogen receptors), glycoprotein complex Ib / V / IX, CD 42 (von Willebrand factor receptor).
- Endomitosis: process in which the cell multiplies its DNA twice without the need to divide, through a process called abortive mitosis. This process is repeated in several cycles. This gives it the property of being a large cell that will produce a lot of platelets..
- Appearance of cytoplasmic processes similar to pseudopods.
Platelets
They are very small structures, measure between 2-3 µm, do not have a nucleus and present 2 types of granules called alpha and dense. Of all the cells mentioned, these are the only ones that can be seen in peripheral blood smears. Its normal value ranges from 150,000 to 400,000 mm3. Its half-life is approximately 8-11 days..
-Thrombocytopoiesis
The mature megakaryocyte will be responsible for forming and releasing platelets. Megakaryocytes, being close to the vascular endothelium in the sinusoids of the bone marrow, form elongations of their cytoplasm, creating a kind of tentacles or pseudopods that are called proplatelets..
The outermost zone of the proplatelets is fragmented to give rise to the platelets. Platelet release occurs in the blood vessels, and is aided by the force of the bloodstream. For this, the proplatelet must cross the endothelial wall.
Some authors claim that there is an intermediate phase between the proplatelet and the platelets that they have called preplatelets. This transformation from propplate to preplate appears to be a reversible process..
Preplatelets are larger than platelets and are discoid in shape. They eventually turn into platelets. Within a few hours, a total of approximately 1,000 to 5,000 platelets will have emerged from a megakaryocyte..
Thrombocytopoiesis stimulants
Stimulating substances include stem cell stimulating factor, interleukin 3, interleukin 6, interleukin 11, and thrombopoietin.
Interleukin 3
This cytokine intervenes by increasing the lifespan of the most primitive and immature stem cells of the megakaryocytic lineage. It does this through the inhibition of the apoptosis or programmed cell death process of these cells..
Interleukin 6
It is a pro-inflammatory interleukin that has various functions in the body. One of its functions is to stimulate the synthesis of hematopoietic precursors, among which is the stimulation of the precursors of the megakaryocytic lineage. It works from the differentiation of the CFU-GEMM to the CFU-meg.
Interlequin 11
Like thrombopoietin, it acts at the level of the entire megakaryocytopoiesis process, that is, from the stimulation of the pluripotential cell to the formation of the megakaryocyte.
Thrombopoietin
This important hormone is synthesized mainly in the liver and secondarily in the kidney and in the stroma of the bone marrow..
Thrombopoietin acts in the bone marrow, stimulating the formation of megakaryocytes and platelets. This cytokine is involved in all phases of megakaryopoiesis and thrombocytopoiesis.
It is believed that it also stimulates the development of all cell lines. It also contributes to the proper functioning of platelets.
Regulation of thrombocytopoiesis
Like any process, thrombocytopoiesis is regulated through certain stimuli. Some will promote the formation and release of platelets into the circulation and others will inhibit the process. These substances are synthesized by cells of the immune system, by the stroma of the bone marrow and by cells of the reticulum endothelial system..
The regulation mechanism keeps the number of platelets at normal levels in the circulation. Approximately daily platelet production is 10eleven.
The stromal microenvironment of the bone marrow plays a fundamental role in the regulation of thrombocytopoiesis.
As the megakaryocyte matures, it moves from one compartment to another; that is, it passes from the osteoblastic compartment to the vascular compartment, following a chemotactic gradient called stromal derived factor - 1.
As long as the megakaryocyte is in contact with components of the osteoblastic compartment (type I collagen), the formation of proplatelets will be inhibited..
It will only be activated when it comes into contact with von Willebrand factor and fibrinogen present in the extracellular matrix of the vascular compartment, together with growth factors, such as vascular endothelial growth factor (VEGF)..
-Thrombopoietin
Thrombopoietin is cleared by platelets when it is taken up through its MPL receptor..
That is why when platelets increase, thrombopoietin decreases, due to high clearance; but when platelets fall, the plasma value of the cytokine rises and stimulates the marrow to form and release platelets.
Thrombopoietin synthesized in the bone marrow is stimulated by the decrease in the number of platelets in the blood, but the formation of thrombopoietin in the liver is only stimulated when the Ashwell-Morell receptor of the hepatocyte is activated in the presence of desialinized platelets..
Desialinized platelets come from the apoptosis process that platelets undergo when they age, being captured and removed by the monocyte-macrophage system at the spleen level..
-Inhibitory factors
Among the substances that slow down the platelet formation process are platelet factor 4 and transforming growth factor (TGF) β.
Platelet factor 4
This cytokine is contained in the alpha granules of platelets. It is also known as fibroblast growth factor. It is released during platelet aggregation and stops megakaryopoiesis.
Transforming growth factor (TGF) β
It is synthesized by various types of cells, such as macrophages, dendritic cells, platelets, fibroblasts, lymphocytes, chondrocytes and astrocytes, among others. Its function is related to the differentiation, proliferation and activation of various cells and also participates in the inhibition of megakaryocytopoiesis.
Diseases produced by imbalance in thrombocytopoiesis
There are many disorders that can alter homeostasis in relation to platelet formation and destruction. Some of them are mentioned below.
Congenital amegakaryocytic thrombocytopenia
It is a strange inherited pathology characterized by a mutation in the thrombopoietin / MPL receptor system (TPO / MPL).
That is why in these patients the formation of megakaryocytes and platelets is almost nil and with time they evolve to a medullary aplasia, which shows that thrombopoietin is important for the formation of all cell lines.
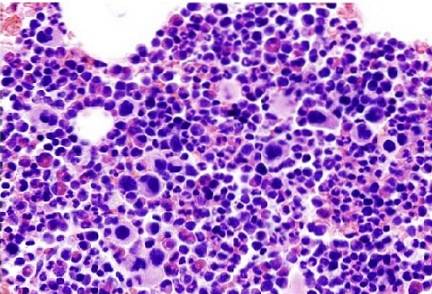
Essential thrombocythemia
It is a rare pathology in which there is an imbalance in thrombocytopoiesis, which causes an exaggerated increase in the number of platelets constantly in the blood and a hyperplastic production of platelet precursors (megakaryocytes) in the bone marrow.
This situation can cause thrombosis or bleeding in the patient. The defect occurs at the level of the stem cell, which is inclined towards the exaggerated production of a cell lineage, in this case the megakaryocytic.
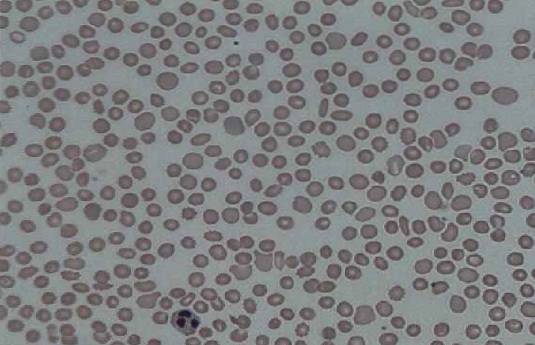
Thrombocytopenia
The reduced number of platelets in the blood is called thrombocytopenia. Thrombocytopenia can have many causes, including: retention of platelets in the spleen, bacterial infections (E. coli enterohemorrhagic) or viral infections (dengue, mononucleosis).
They also appear due to autoimmune diseases, such as systemic lupus erythematosus, or of drug origin (treatments with sulfa drugs, heparin, anticonvulsants).
Other probable causes are decreased platelet production or increased destruction of platelets..
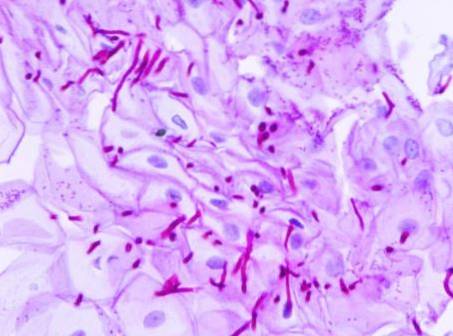
Bernard-Soulier syndrome
It is a rare hereditary congenital disease. It is characterized by presenting platelets of abnormal morphology and function caused by a genetic alteration (mutation), where the von Willebrand factor receptor (GPIb / IX) is absent.
Therefore, clotting times are increased, there is thrombocytopenia and the presence of circulating macroplates..
Immune thrombocytopenic purpura
This pathological condition is characterized by the formation of autoantibodies against platelets, causing their early destruction. As a consequence, there is a significant decrease in the number of circulating platelets and a low production of them..
References
- Heller P. Megakaryocytopoiesis and thrombocytopoiesis. Physiology of normal hemostasis. 2017; 21 (1): 7-9. Available at: sah.org.ar/revista
- Mejía H, Fuentes M. Immune thrombocytopenic purpura. Rev Soc Bol Ped 2005; 44 (1): 64 - 8. Available at: scielo.org.bo/
- Bermejo E. Platelets. Physiology of normal hemostasis. 2017; 21 (1): 10-18. Available at: sah.org.ar
- Saavedra P, Vásquez G, González L. Interleukin-6: friend or foe? Bases to understand its usefulness as a therapeutic objective. Iatreia, 2011; 24 (3): 157-166. Available at: scielo.org.co
- Ruiz-Gil W. Diagnosis and treatment of immunological thrombocytopenic purpura. Rev Med Hered, 2015; 26 (4): 246-255. Available at: scielo.org
- "Thrombopoiesis." Wikipedia, The Free Encyclopedia. 5 Sep 2017, 20:02 UTC. 10 Jun 2019, 02:05 Available in: es.wikipedia.org
- Vidal J. Essential thrombocythemia. Protocol 16. Hospital Donostia. 1-24. Available at: osakidetza.euskadi.eus


Yet No Comments