
Volemia what indicates, how is it calculated, variations

Volemia is a technical term used in medical jargon to refer to the volume of whole blood contained in the cardiovascular system. It is an expression made up of the first letters of the word volume and the word "emia”Which comes from the Greek“ haemia ”and refers to blood.
Blood volume can be determined by various methods and estimated based on body weight. It is important that it stays within a certain range, since significant changes in its volume can modify blood pressure or the composition of circulating fluids..
The body has regulatory mechanisms that are activated by changes in the volume and composition of the circulating volume, triggering behavioral and hormonal mechanisms that allow maintaining said volume within normal ranges..
The normal values of blood volume in men vary between 70 and 75 ml / Kg of body weight, while in women it is between 65 and 70 ml / Kg of body weight.
Article index
- 1 What does blood volume indicate?
- 2 How is it calculated?
- 3 Distribution
- 4 Variations
- 4.1 Hypovolemia
- 4.2 Hypervolemia
- 5 Regulation
- 6 References
What does volemia indicate?
Although the meaning of the word seems clear from the previous definition, it is important to insist on what the term indicates, especially when it is also defined as "the volume of circulating blood" and can be confused with another medical technical term such as the "cardiac output".
Cardiac output is the volume of blood driven by the heart in a unit of time. It is a dynamic concept. Its magnitude is expressed in units of volume / time (L / min). That volume flows in one minute through the entirety of each circuit and returns to the heart to recirculate again.
Vollemia, on the other hand, is the amount of whole blood that occupies the cardiovascular bed, regardless of whether it moves or not and the rate at which it moves. Its magnitude may have hemodynamic repercussions, but it is simply a volume and is more of a static concept.
The difference is better understood when one thinks of a person with a blood volume of 5 liters who, at rest, maintains a cardiac output of 5 L / min, but with moderately intense exercise increases his output to 10 L / min. In both cases the blood volume was the same, but the cardiac output doubled.
How is it calculated?
The blood volume in a person can be determined using estimation methods for which indices related to body weight are used. Although with technically more complicated laboratory procedures a much more exact measurement can also be performed.
Estimation methods do not measure actual blood volume, but rather estimate what the normal value of that variable should be. It is assumed for this that, in an adult male, the blood volume should be (in liters) 7% of his body weight (in kilos), or also that for each Kg of weight he will have 70 ml of blood.
Using the dilution principle, two methods can be used to measure the volume of blood in the body. With the first, this volume is directly deduced; with the second, the plasma volume and hematocrit are measured separately and from them the total blood volume is calculated.
To measure the volume of a liquid using the dilution principle, a known quantity of an indicator (Mi) is administered that is evenly distributed in that liquid; A sample is then taken and the concentration of the indicator (Ci) is measured. Volume (V) is calculated using V = Mi / Ci.
In direct volume measurement, red blood cells radioactively labeled with 51 Cr are injected and the radioactivity of a sample is then measured. For the second method, the plasma volume is measured using Evans Blue or radioactive albumin (125I-albumin), and the hematocrit.
In the latter case, the total blood volume (Vsang) is calculated by dividing the plasma volume (VP) by 1 - Hematocrit (Ht), expressed as a fraction of the unit and not as a percentage. That is: Vsang = VP / 1 - Hto.
Distribution
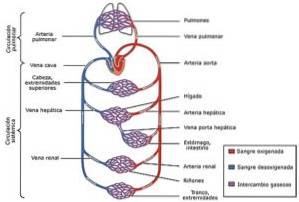
The blood volume in a 70 kg man (7% of that weight) would be around 5 liters (4.9), 84% contained in the systemic circulation, 7% in the heart and 9% in the pulmonary vessels. Of the 84% systemic: 64% in veins, 13% in arteries and 7% in arterioles and capillaries.
Variations
Although the value of blood volume must be kept within certain limits (normovolemia), situations may arise that tend to modify it. Such situations can lead to a reduction (hypovolaemia) or an increase (hypervolaemia) in blood volume..
Hypovolemia
Hypovolemia can be caused by complete blood loss as in hemorrhages; by reducing the blood fluid component due to water deficit as in dehydration or by accumulation of water in fluid compartments other than the intravascular.
Causes of dehydration can be diarrhea, vomiting, heavy sweating, exaggerated use of diuretics, diabetes insipidus with exaggerated diuresis. The accumulation of water in different compartments occurs in the interstitium (edema), the peritoneal cavity (ascites) and the skin (severe burns).
Hypovolemia can be accompanied by a series of dehydration symptoms such as thirst, dry skin and mucous membranes, hyperthermia, weight loss, and sagging skin. Other symptoms include tachycardia, weak pulse and arterial hypotension and, in extreme cases, even hypovolemic shock..
Hypervolemia
Hypervolemia can occur due to water intoxication when the intake of water exceeds its excretion. Retention may be due to an exaggerated antidiuretic hormone (ADH) secreting tumor. ADH induces exaggerated reabsorption of water in the kidney and reduces its excretion.
Heart and kidney failure, liver cirrhosis, nephrotic syndrome and glomerulonephritis, as well as compulsive and exaggerated fluid intake in some mental illnesses or exaggerated administration of parenteral solutions are also causes of hypervolemia..
Symptoms of hypervolemia include those related to increased blood pressure and cerebral edema, such as headache, vomiting, apathy, altered consciousness, seizures, and coma. Fluid can build up in the lungs (pulmonary edema).
Regulation
The blood volume must be kept within certain limits considered normal. The body is subject to normal or pathological circumstances that tend to modify these values, but it has control mechanisms that tend to counteract these changes..
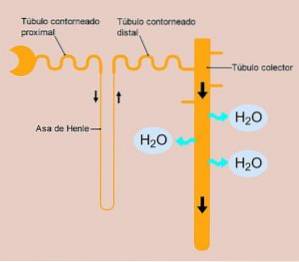
Control systems imply the existence of sensors that detect variations and structures that coordinate responses. The latter include modifying fluid intake through the thirst mechanism and modifying renal water excretion through ADH..
Volume variations are detected by pressure receptors in arteries (aorta and carotid) and in pulmonary vessels and atria. If blood volume increases, receptors are activated, the thirst mechanism is inhibited, and less fluid is ingested.
Activation of pressoreceptors in hypervolemia also inhibits ADH secretion. This hypothalamic hormone released in the neurohypophysis promotes renal reabsorption of water and reduces its excretion. Its absence favors the urinary elimination of water and reduces hypervolemia.
Another stimulus involved in controlling blood volume is plasma osmolarity. If decreased (hyposmolar hypervolaemia), osmoreceptors in the hypothalamus are inactivated and thirst and ADH secretion are inhibited, thereby lowering plasma volume and blood volume.
Hypovolemia and plasma hyperosmolarity have opposite effects to those just mentioned. Pressoreceptors are inactivated and / or osmoreceptors are activated, which triggers thirst and ADH is secreted, which ends with water retention at the renal tubular level and blood volume increases..
References
- Ganong WF: Central Regulation of Visceral Function, in Review of Medical Physiology, 25th ed. New York, McGraw-Hill Education, 2016.
- Guyton AC, Hall JE: The Body Fluid Compartments: Extracellular and intracellular fluids; Edema, in Textbook of Medical Physiology, 13th ed, AC Guyton, JE Hall (eds). Philadelphia, Elsevier Inc., 2016.
- Huether SE: The Cellular environment: Fluids and Electrolytes, acids and bases, in Pathophysiology, The Biologic Basis for Disease in Adults & Children, 4th ed, KL McCance and SE Huether (eds). St. Louis, Mosby Inc., 2002.
- Persson PB: Wasser-und Elektrolythaushalt, in Physiologie des Menschen mit Pathophysiologie, 31th ed, RF Schmidt et al (eds). Heidelberg, Springer Medizin Verlag, 2010.
- Zideck W: Wasser- und Electrolythaushalt, in Klinische Pathophysiologie, 8th ed, W Siegenthaler (ed). Stuttgart, Georg Thieme Verlag, 2001.



Yet No Comments