
Müeller Hinton agar foundation, preparation and uses
The Müeller Hinton agar It is a solid, non-selective nutrient medium that is composed of meat infusion, acid casein peptone, starch, agar and distilled water. This medium allows excellent microbial growth of most fast growing bacteria.
It was originally created by John Howard Müeller and Jane Hinton to isolate nutritionally demanding bacteria such as Neisseria gonorrhoeae Y Neisseria meningitidis. However, due to its characteristics, it turned out to be ideal for the study of susceptibility to antibiotics, providing reliable and reproducible results..

For this reason, Müeller Hinton agar is the culture medium accepted by the Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing, for the performance of the antimicrobial susceptibility test by the Kirby disk diffusion method and Bauer.
Article index
- 1 Rationale
- 2 Preparation
- 3 Uses
- 3.1 The antibiogram technique
- 3.2 Strategic placement of discs on Müeller Hinton agar
- 4 Causes of erroneous results
- 5 Limitation
- 6 Quality control
- 7 References
Basis
As it is a non-selective nutritive medium, it is excellent for the growth of most pathogenic bacteria..
On the other hand, its simple composition makes the substances easily diffuse on it, being an essential characteristic for the susceptibility test by the disk diffusion method..
Another of its characteristics is that it contains a low amount of inhibitors, which allows sulfonamides, trimethoprim and tetracyclines to be evaluated effectively..
However, it must be borne in mind that the medium must meet certain conditions to ensure its proper functioning, including:
The adjustment of the pH, the depth of the agar and the appropriate concentration of thymine, thymidine, Ca++, Mg++ and Zn++.
You also have to know that the methodology is standardized and therefore all the parameters must be met, such as:
The inoculum concentration, the concentration and conservation of the antibiotic discs, the placement of the appropriate number of discs on the agar, the distance between one disc and another, the strategic placement of certain antibiotics, the atmosphere, the temperature and the time of incubation.
Preparation
Weigh out 37 g of dehydrated Müeller Hinton medium and dissolve in 1 liter of distilled water. Heat the medium while stirring to aid dissolution. Boil for 1 minute.
Autoclave to sterilize at 121 ° C for 15 minutes. When removing from the autoclave, the flask should be placed in a water bath at 50 ° C to cool. Pour 25 to 30 ml into sterile 10 cm diameter Petri dishes.
The plates should be with an average thickness of 4 mm (ideal), being allowed a range of 3-5 mm.
If it is desired to prepare blood agar using Müeller Hinton agar as a base, pour 5% sterile and defibrinated lamb blood before serving on the plates..
The final pH of the medium should be between 7.2 to 7.4.
Invest and store in the refrigerator, until use. Allow the plate to come to room temperature before use.
The color of the prepared medium is light beige.
Applications
Used to perform antibiogram or antibiotic susceptibility testing for most fast growing non-fastidious pathogens.
If the agar is supplemented with blood, it is used to carry out the antibiogram of demanding microorganisms such as: Streptococcus pneumoniae, Haemophilus sp, Neisseria meningitidis, among others. It has also been used to isolate Legionella pneumophila.
Antibiogram technique
Before performing the antibiogram, a bacterial solution equivalent to 1.5 x 10 must be prepared.8 cells.
For this, 3 to 4 colonies of the pure culture are taken and suspended in a soybean trypticase broth or in Müeller Hinton broth, incubated for 2 to 6 hours and the concentration is adjusted with sterile saline, comparing it with a Mac Farland standard of 0.5%.
If they are demanding microorganisms, colonies can be suspended directly up to the concentration of 0.5% Mac Farland. Subsequently, the Müeller Hinton plate is sown with a swab impregnated with the prepared bacterial solution..
To do this, the swab is immersed in the solution and then excess liquid is removed by pressing against the walls of the tube. Immediately afterwards, the swab is passed over the entire surface, leaving no places untouched, then the plate is slightly rotated and it is seeded again. The operation is repeated 2 more times.
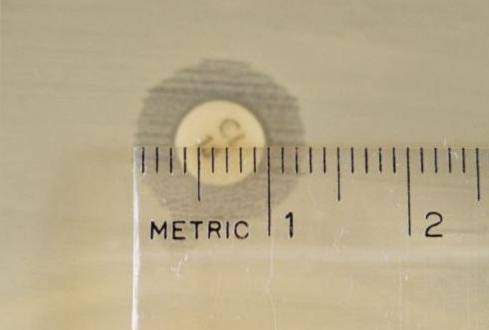
Allow to stand for 10 minutes and then attach the antibiotic discs with a sterile forceps, leaving a 24mm gap between them. After placing each disc on the agar, press each disc lightly with the forceps to ensure that they are well adhered..
Once the process is finished, the plate is inverted and incubated at 35-37 ° C in aerobiosis for 16 to 18 hours. If it is a demanding microorganism, it may warrant microaerophilia and if the antibiogram contains oxacillin discs, it should be read after 24 hours..
A ruler is used to measure the diameter of each halo. The results should be recorded in mm. Subsequently, the values obtained are correlated with the cut point tables published by the current CLSI manual..
Report as sensitive (S), intermediate (I), or resistant (R), as the case may be.
Antibiotics are selected according to the isolated microorganism and the type of infection that is causing.
Sometimes the strategic placement of antibiotics must be taken into account to show phenotypic patterns of resistance.
Strategic placement of discs on Müeller Hinton agar
For enterobacteria, the clavulanic acid disc should be placed against 3rd and 4th generation cephalosporins. An egg-shaped broadening indicates that the strain is a producer of extended-spectrum beta-lactamases (ESBL). This means that the patient should not be treated with any cephalosporins..

In Staphylococcus it is important to place the erythromycin or azithromycin disc in front of the clindamycin disc (D-test).
A resistant halo in erythromycin and a flattening in the clindamycin halo indicates that the strain possesses strain inducible clindamycin resistance (ICR). This means that a treatment with clindamycin will not be effective..
To search for inducible AMP C strains in Enterobacteriaceae and some non-fermenting Gram negative rods, ceftazidime, cefoxitin or piperacillin tazobactan discs are faced against an imipenem disc, at a distance of 27 mm.
A flattened halo in one of the discs facing imipenem indicates the presence of inducible AMP C.
For the search for constitutive C-AMP, a 500 µg cloxacillin disk is faced with ceftazidime (30 µg) and with cefotaxime (30 µg), at a distance of 25 mm. A widened halo in any of the cephalosporins indicates positivity.
The cloxacillin disk can also be replaced by a 9 mm disk of Whatman No. 6 filter paper impregnated with phenyl boric acid (400 µg) with a distance of 18 mm. It is interpreted the same as the previous one.
Finally, to investigate the production of metallobetalactamases especially in Pseudomonas aeruginosa, A disc impregnated with 10 µl of ethylenediaminetetraacetic acid (EDTA 750 µg) and thioglycolic acid (SMA 300 µg) is used, which faces the imipenem and meropenem discs, at a distance of 15 mm.
The test is positive if there is widening of the imipenem or meropenem halos towards the EDTA / SMA disk. This result must be confirmed by the modified Hodge test..
This method consists of inoculating a strain of Escherichia coli ATCC 25922 on the Müeller Hinton plate. An imipenem disk is placed in the center of the plate and then a streak is made from the disk towards the periphery with the strain of P. aeruginosa suspicious. Up to 4 strains can be tested per plate.
The test will be positive if there is a zone of distortion of the imipenem halo around the stretch mark.
Causes of erroneous results
-Poorly preserved antibiotic discs can produce false resistance. For example, the oxacillin disk is very vulnerable to changes in temperature..
-A pH of the medium below that indicated (acidic) produces smaller halos in aminoglycosides and macrolides (risk of false resistance), and larger halos in penicillin, tetracycline and novobiocin (risk of false sensitivity).
-If the pH is above that indicated (alkaline) the effects described above are reversed.
-Media with elevated thymine and thymidine concentrations have an influence by significantly reducing the inhibition halos of sulfonamides and trimethoprim.
-High concentrations of calcium and magnesium produce false resistance of aminoglycosides, polymyxin B and tetracyclines against strains of Pseudomonas aeruginosa.
-Low concentrations of calcium and magnesium produce false sensitivities of aminoglycosides, polymyxin B and tetracyclines against strains of Pseudomonas aeruginosa.
-The presence of zinc affects the results of carbapenem discs (imipenem, meropenem and ertapenem).
-Media thickness below 3mm will produce false sensitivity results, while thickness above 5 will produce false resistance.
-The mobilization of discs in the antibiogram will give deformed halos, since the discharge of antibiotics is immediate.
- Very weak inoculums affect the results, since there will not be a uniform or confluent growth in the agar, a necessary condition to be able to measure the inhibition halos, in addition to that the halos can give larger than normal.
-Overly charged inoculums can give smaller than normal halos.
-Not respecting the distance between discs causes one halo to overlap with another and they cannot be read correctly.
-Incubate with COtwo increases the size of the halos of the tetracycline and methicillin discs.
-Incubate at temperatures below 35 ° C produces larger halos.
-The addition of blood decreases the size of the sulfonamide halo.
Limitation
The sensitivity of an antibiotic demonstrated in the antibiogram against a microorganism (in vitro) is no guarantee that it will work in vivo.
QA
To know if the medium contains the adequate amount of thymine, a strain must be grown Enterococcus faecalis ATCC 29212 and test the susceptibility to trimethoprim sulfamethoxazole (SXT), it must give a halo equal to or> 20 mm to be satisfactory.
References
- "Müller-Hinton agar." Wikipedia, The Free Encyclopedia. 16 Nov 2018, 12:23 UTC. 27 Jan 2019, 04:22
- Forbes B, Sahm D, Weissfeld A. (2009). Bailey & Scott Microbiological Diagnosis. 12 ed. Editorial Panamericana S.A. Argentina.
- Cona E. Conditions for a good susceptibility study by agar diffusion test. Rev Chil Infect, 2002; 19 (2): 77-81
- Difco Francisco Soria Melguizo Laboratory. Müeller Hinton agar with 5% sheep blood. 2009.Available at: http://f-soria.es
- BD Müeller Hinton II Agar Laboratory. 2017.Available at: .bd.com
- Britannia Laboratories. Müeller Hinton agar. 2015.Available at: britanialab.com
- Koneman E, Allen S, Janda W, Schreckenberger P, Winn W. (2004). Microbiological Diagnosis. 5th ed. Editorial Panamericana S.A. Argentina.
- Martínez-Rojas D. AmpC-type betalactamases: Generalities and methods for phenotypic detection. Rev. Soc. Ven. Microbiol. 2009; 29 (2): 78-83. Available at: scielo.org.
- Perozo A, Castellano M, Ling E, Arraiz N. Phenotypic detection of metallobetalactamases in clinical isolates of Pseudomonas aeruginosa. Kasmera, 2012; 40 (2): 113-121. Available at: scielo.org.


Yet No Comments