
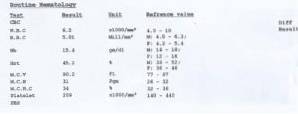
Hematic biometry description, normal values, examples
The hematic biometry, Also known as a blood count, it is a complete count of blood cells such as red blood cells, white blood cells, and platelets. Likewise, it reports the hemoglobin values and some related variables. All this in order to provide detailed information on the patient's health status
Hemoglobin is a protein found within the red blood cell that is responsible for the transport of oxygen in the bloodstream. Normal hemoglobin concentrations are therefore vitally important for health.

Related to hemoglobin, the hematic biometry reports the mean corpuscular hemoglobin and the mean corpuscular hemoglobin concentration. Regarding the red blood cells (RBC), the hematocrit or percentage of RBC by volume and the mean corpuscular volume are also evaluated..
The hematic biometry is very important as a paraclinical examination, since many pathological conditions present with hematic alterations. For example, a significant decrease in the numbers of red blood cells and / or hemoglobin is related to anemias, infectious processes can occur with increases in white blood cells.
Atopic or allergic processes are accompanied by increases in some particular types of white blood cells, and some coagulation disorders, of infectious origin (dengue) or not, can lead to a decrease in platelet counts.
Article index
- 1 Description
- 1.1 - Red series
- 1.2 - Leukocytes
- 1.3 - Platelets
- 2 Normal values
- 3 Examples
- 4 References
Description
The hematic biometry is also called hemogram or hematic cytometry and is one of the laboratory studies requested most frequently by the clinician, both for outpatients and hospitalized patients.
It is a test that assesses the three cell lines produced by the bone marrow: erythrocytes or red blood cells, leukocytes or white blood cells, and platelets. Requires a venous blood sample that is drawn in aseptic and antiseptic conditions from a fasting patient.
- Red series
First, the red series is reported, which is made up of the primary and secondary red cell indices. Primary ones include red blood cell count, hemoglobin concentration, and hematocrit..
The secondary red cell indices are calculated based on the primary ones and include the mean corpuscular hemoglobin (HGM), the mean blood cell volume (VGM) and the mean concentration of corpuscular or globular hemoglobin (CMHG).
The red series allows the diagnosis of normality, polycythemia or anemia, and indicates the size and hemoglobin content of the erythrocytes studied.
Secondary red cell indices are calculated as follows:
Mean globular hemoglobin concentration
CMHG = Hemoglobin x 100 / hematocrit
Medium corpuscular volume
VGM = Hematocrit x 10 / number of erythrocytes per microliter
Mean globular hemoglobin
HGM = Hemoglobin x 10 / number of erythrocytes per microliter
- Leukocytes
The assessment of leukocytes or white blood cells includes three determinations: the total count, the differential count, and the differential count in neutrophils, called the Schilling differential count..
The differential count includes the percentage of each type of leukocyte stained with a Wright stain from a sample from a smear of 100 leukocytes. The differential Schilling count is made in the sample of 100 leukocytes from neutrophils.
The types of leukocytes reported are lymphocytes, monocytes, basophils, eosinophils, neutrophils, segmented, non-segmented, metamyelocytes, myelocytes, and promyelocytes. They are reported in percentage and absolute values. The myeloid series is not always reported.
- Platelets
Platelets are reported in absolute numbers per unit volume.
Normal values
- Erythrocytes
Women: 4.2 to 5.4 million cells / µl of blood.
Men: 4.7 to 6.2 million cells / µl of blood.
- Platelet count
150,000 to 400,000 units / µl of blood.
- Hemoglobin
Women: 12.1 to 15.1 g / dl or 7.5 to 9.36 mmol / L.
Men: 13.8 to 17.2 g / dL or 8.56 to 10.66 mmol / L.
- Hematocrit
Women: 36.1 to 44.3%
Men: 40.7 to 50.3%
- CMHG
30 to 37%
- VGM
80 to 95 fl (femtoliters)
- HGM
24 to 34 pg (picograms)
- Leukocytes
4,500 to 11,000 cells / µl of blood
- Lymphocytes
1,300 to 4,000 cells / µl of blood (20 to 50%).
- Neutrophils
1,500 to 8,000 cells / µl of blood (35 to 70%).
- Neutrophils sec.
2500 to 7500 cells / µl of blood (90 to 100%).
- Neutrophils no sec.
10 to 20 cells / µl of blood (0 to 10%).
- Eosinophilsgm
60 to 500 cells / µl of blood (0 to 5%).
- Basophils
10 to 150 cells / µl of blood (0 to 2%).
- Monocytes
150 to 900 cells / µl of blood (0 to 10%).
Hematic biometry provides information on the absolute or relative numbers of the different types of blood cells, as well as various structural and functional characteristics of them..
Deviations from normal values can reflect diseases, physiological states (such as pregnancy, childhood or old age), injury or dysfunction of almost any part of the body.
Examples
An altered number of red blood cells can be the result of erythropoietic (red blood cell production system) dysfunctions, anemias, hemorrhages, Hodgkin's disease, or leukemia. Changes in the VGM or MCV that show the size of red blood cells are seen in anemias and thalassemias.
The HGM (MCH in English) that shows the amount of hemoglobin in each erythrocyte (by weight) is altered in anemia and hemoglobinopathies (diseases that present with alterations in the structure of hemoglobin).
The CMHG (MCHC in English) is the concentration of hemoglobin in each erythrocyte expressed as a percentage and is altered in anemias and spherocytosis. The latter is a hereditary disease that causes hemolytic anemia due to destruction of red blood cells and the presence of spherocytes in the blood, which are round erythrocytes.
The hematocrit represents the volume that red blood cells occupy in a given volume of blood and expressed as a percentage. This is modified outside the normal ranges in anemias, erythrocytosis, hemorrhages and leukemias, among others.
Hemoglobin values are modified in anemias, which are diseases that occur with a decrease in the production of red blood cells or with a decrease in the production of hemoglobin, generally due to iron deficiency, which is why hemoglobin in the blood decreases.
Leukocytes and their differential count are modified in many pathological processes, the most frequent being infectious processes. The increase in the number of leukocytes in the blood is called leukocytosis and its decrease is called leukopenia.
The number of circulating platelets can be altered in many pathological conditions such as some infectious processes such as dengue, hemolytic diseases of the newborn, multiple myeloma, leukemias, etc..
References
- Chandra, S., Tripathi, A. K., Mishra, S., Amzarul, M., & Vaish, A. K. (2012). Physiological changes in hematological parameters during pregnancy. Indian journal of hematology and blood transfusion, 28(3), 144-146.
- Ganong, W. F., & Barrett, K. E. (2012). Ganong's review of medical physiology. McGraw-Hill Medical.
- Gaona, C. A. (2003). Interpretation c station c clinical station of hematic biometry clinical of hematic biometry. University Medicine, 5(18), 35.
- López-Santiago, N. (2016). Hematic biometry. Acta pediátrica de México, 37(4), 246-249.
- McCance, K. L., & Huether, S. E. (2018). Pathophysiology-EBook: The Biologic Basis for Disease in Adults and Children. Elsevier Health Sciences.
- Piedra, P. D., Fuentes, G. O., Gómez, R. H., Cervantes-Villagrana, R. D., Presno-Bernal, J. M., & Gómez, L. E. A. (2012). Determination of reference intervals clinical blood count in the Mexican population. Latin American Journal of Clinical Pathology and Laboratory Medicine, 59(4), 243-250.
- Wagner, M., Krueger, G. R., Abrlashi, D. V., Whitman, J. E., & Rojo, J. (1998). Chronic fatigue syndrome (CFS): Review of clinical data from 107 cases. Rev. medic. Hosp. Gen. Mex, 61(4), 195-210.


Yet No Comments