
Amsel criteria

The Amsel criteria are the four characteristics or clinical principles that must be present in order to establish the clinical diagnosis of bacterial vaginosis. It should not be confused with the Nugent criteria; Although they fulfill the same diagnostic objective, the latter are based only on microbiological findings in the laboratory.
To establish the diagnosis of bacterial vaginosis using the Amsel criteria, at least three of the four criteria must be present in the patient simultaneously; otherwise, the symptoms may be due to similar non-bacterial pathologies.
Vulvovaginal discomfort is one of the most frequent pathologies in the area of gynecology, and infections in the vagina and vulva tend to express similar symptoms that make their recognition difficult in the patient..
Of these discomforts, changes in vaginal discharge are the most frequent reason for consultation, and although they do not always have a pathological connotation, each time this symptom appears, the etiopathogenesis must be evaluated and clarified..
Bacterial vaginosis is considered the most predominant etiology in women of reproductive age. Although it is not considered a sexually transmitted infection, it has been shown to contribute to their spread.
Article index
- 1 Physiological characteristics of the vagina
- 1.1 Complications
- 2 Amsel criteria
- 2.1 Appearance of vaginal discharge
- 2.2 vaginal pH greater than 4.5
- 2.3 Positive amine test (KOH 10%)
- 2.4 Presence of desquamation cells
- 3 References
Physiological characteristics of the vagina
Under normal conditions, vaginal pH is acidic thanks to the action of Döderlein bacilli, which produce lactic acid, causing the pH to remain at 4 in women of childbearing age.
The bacterial microbiota, despite being quite dynamic and diverse, also remains in perfect balance when conditions permit..
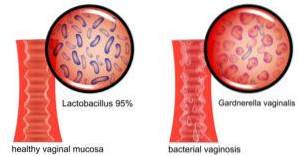
The vaginal saprophytic bacterial flora consists predominantly of Lactobacillus spp, with the prevalent species L. crispatus, L. acidophilus Y L. gasseri, and they are in charge of acting as defenders of some pathogenic microorganisms.
The pathophysiological mechanism has not yet been perfectly described; However, it can be said that it is basically a replacement of that saprophytic flora by pathogenic germs such as Gardnerella vaginalis, Mobiluncus spp, Porphyromonas spp, Prevotella spp, among others.
There are some factors that can influence the balance of the saprophytic bacterial flora. These factors can be endogenous, such as the stage of the menstrual cycle in which the patient is or age; or exogenous, such as some drugs or contact with detergents in lingerie.
Complications
Bacterial vaginosis is not considered a bacterial vaginitis, since on electron microscopy no leukocytes or porlimorphonuclear cells are found in the vaginal discharge; therefore, it is not an inflammatory process.
This type of infection is frequently associated with a considerable increase in the risk of preterm delivery due to premature rupture of membranes, choriamionitis, puerperal and neonatal sepsis..
These infections are also associated with promoting the establishment of cervical intraepithelial neoplasia (CIN). Severe infections can cause acute contiguous salpingitis,
Amsel criteria
The Amsel criteria are four. In order to establish the clinical diagnosis of bacterial vaginosis, at least three of the four parameters must be met..
This requires taking a sample of vaginal discharge with a sterile swab. According to the study of the discharge, the following will be confirmed:
Appearance of vaginal discharge
The vaginal discharge takes on a milky, homogeneous, grayish or yellowish appearance, called leucorrhoea. In some cases it is smelly.
The difference between bacterial vaginosis and other pathologies that cause leukorrhea is very difficult to establish, especially due to the subjectivity in the observation of vaginal discharge.
In fact, in some cases the change between the vaginal discharge considered "normal" in some patients is very subtle, and can be confused with the thick vaginal discharge characteristic of the end of the menstrual cycle due to the increase in progesterone.
About 50% of patients with bacterial vaginosis do not notice a difference in vaginal discharge, especially pregnant women.
vaginal pH greater than 4.5
On some occasions the pH can be elevated if there is presence of remains of menstrual bleeding, cervical mucus or semen after sexual intercourse; therefore, it is not such a specific criterion on its own for the diagnosis of vaginosis.
Positive amine test (KOH 10%)
It is also known as "the smell test"; Despite being a fairly specific criterion, it is not very sensitive. This means that, although whenever it gives a positive result it will indicate the presence of bacterial vaginosis, not every time the infection is established it will be positive.
This test consists of adding a drop of 10% potassium hydroxide to the vaginal discharge sample. If a foul odor begins to appear (some literatures describe it as a fishy odor), the amine test result is considered positive.
This happens because, when potassium hydroxide comes into contact with vaginal discharge, the release of amines immediately occurs, leading to the appearance of a foul odor. If no foul odor appears, it is thought of a non-bacterial infection, and suggests a possible candidiasis.
Presence of flaking cells
The presence of scaly cells corresponds to the most specific and sensitive criteria for establishing the diagnosis of bacterial vaginosis..
These are desquamated epithelial cells covered by coccobacilli that are clearly evident in electron microscopy, and that practically establish the diagnosis on their own.
The Amsel criteria alone cannot establish an accurate diagnosis due to the subjectivity in the observation of vaginal discharge and the various physiological states that can lead to the appearance of these criteria. However, the presence of three criteria establishes an accurate diagnosis in 90% of cases..
References
- Egan ME, Lipsky MS. Diagnosis of vaginitis. Am Fam Physician. 2000 Sep 1 Recovered from: ncbi.nlm.nih.gov
- Amsel R, Totten PA, Spiegel CA, Chen KC, Eschenbach D, Holmes KK. Nonspecific vaginitis. Diagnostic criteria and microbial and epidemiologic associations. Am J Med. 1983 Jan Recovered from: ncbi.nlm.nih.gov
- Nicolas Pérez. Bacterial vaginosis and threatened preterm labor. Escuintla Regional National Hospital. July-December 2010. Recovered from: library.usac.edu.gt
- VESPERO, E. C .; AZEVEDO, E. M. M .; Pelisson, M .; PERUGINI, M. R. E. Correlation between clinical criteria and non-diagnostic laboratory criteria of bacterial vaginose. Semina: Ci. Biol. Saúde. Londrina, v. 20/21, n. 2 P. 57-66, Jun. 1999/2000. Recovered from: uel.br
- Melissa Conrad. Bacterial Vaginosis. Recovered from: medicinenet.com



Yet No Comments