
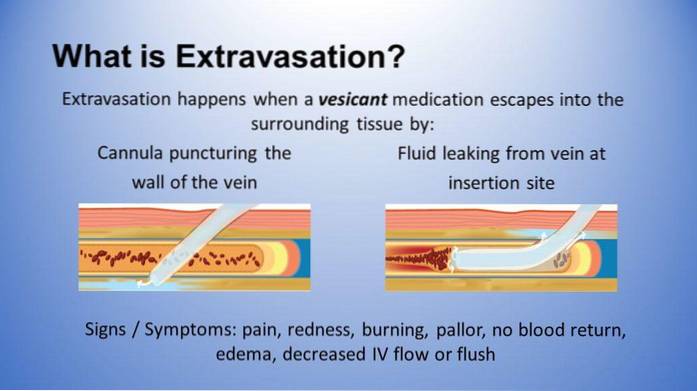
Extravasation signs and management

The extravasation it is the leakage of fluid from a blood vessel into the extravascular space, either into the cell or into the interstitium. This phenomenon can occur with the normal content of the vessel (plasma) or with any medication, drug, mixture or solution that is being administered to a patient intravenously..
There are many causes to explain the leakage of fluid from the vessels to the outside. In most cases it is due to a systemic disease that alters the endothelium or plasma proteins, although damage to a vein due to the presence of a misplaced catheter or the administration of a highly irritating drug can also cause it..
Precociously diagnosing the extravasation of any drug is of vital importance for the well-being of the patient. If the drug is very toxic it can cause tissue damage and necrosis; In addition, the leakage of the drug would imply that the patient is not receiving the treatment in an adequate way, which would delay their improvement.
Article index
- 1 Signs
- 1.1 Plasma extravasation
- 1.2 Drug extravasation
- 2 Management of extravasation
- 2.1 Management of endothelial damage
- 2.2 Management of hypoalbuminemia
- 2.3 Management of cytostatic extravasation
- 2.4 Management of non-cytostatic drug extravasation
- 3 Mucocele due to extravasation
- 4 References
Signs
Depending on the cause, the signs and symptoms of extravasation may vary. As already explained, there is extravasation of the usual intravascular fluid or of some medication that is being administered. Each of these is explained and described below:
Plasma extravasation
The leakage of the normal contents of the blood vessel is associated with endothelial damage or hypoalbuminemia. In turn, there are many causes related to these two events, but the symptoms of each one is common regardless of the cause..
Endothelial damage
The innermost wall of the blood vessels, which fulfills many functions, can be altered for various reasons. Risk factors for endothelial dysfunction include:
- Cigarette smoking.
- Old age.
- Arterial hypertension.
- Dyslipidemia.
- Hyperglycemia.
- Trauma.
- Immune diseases.
When there is chronic endothelial injury, fluid extravasation is incipient. The patient may manifest a slight increase in volume in the affected area, without intense pain or local heat.
There is also usually no functional limitation, or at least not significantly. When the damage is acute, as in trauma, if there may be signs of inflammation.
Hypoalbuminemia
Without being a habitual condition, when it is present it can be dramatic. Among the most important causes of hypoalbuminemia are the following:
- Nephrotic syndrome.
- Malnutrition.
- Liver failure.
The extravasation associated with the decrease in albumin is due to the loss of oncotic pressure; In these circumstances, the pores of the vessels open and allow the plasma to escape. Depending on serum protein levels, fluid leakage will be limited or massive.
The edema associated with extravasation due to hypoalbuminemia is hard; it is cold to the touch and leaves fovea. It always begins with the lower limbs and can progress to the anasarca.
Pleural effusion is even common, and other symptoms such as dyspnea, muscle weakness, arthralgia, cramps, fatigue and loss of appetite may appear..
Drug extravasation
Although not all drugs that are extravasated cause massive tissue damage, they all cause significant discomfort. The management will then depend on the toxicity of the drug and the associated symptoms..
Cytostatic drug extravasation
Cancer or chemotherapy drugs are the most toxic substances that are usually extravasated. Some authors describe this as a serious complication of antineoplastic treatment, ranging between 0.6 and 1.5% incidence, and which can cause chronic and irreversible damage.
Pain is the first warning sign. Patients describe it as excruciating, burning, very intense pain that can radiate to the rest of the affected limb and does not subside even when the infusion is stopped. Immediately, the skin color change, edema and local heat appear..
Later the most severe complications begin. Due to their functions, chemotherapy drugs cause enormous cellular damage; the affected tissue is devitalized in a few minutes and necrosis can spread if corrective measures are not taken immediately. Ulceration is common and, due to obvious immunosuppression, infections appear.
Non-cytostatic drug extravasation
Although they do not cause the same damage as antineoplastic drugs, they also have dire consequences. As described in the previous section, pain is the first symptom that occurs when the drug is misplaced..
Then local redness may be evidenced and an increase in temperature in the affected area is also usual..
This condition does not immediately progress to necrosis, but it can be complicated by infections. However, when the amount of extravasated drug is abundant, regional blood flow can be compromised and cell death may be promoted..
Extravasation management
Extravasation associated with endothelial damage or hypoalbuminemia should be managed according to the cause..
Management of endothelial damage
The treatment is very similar to that used in patients with high cardiovascular risk. It is based on antihypertensives, statins, oral hypoglycemic and anti-inflammatory drugs.
Lifestyle changes, such as quitting smoking and eating healthier, are permanent recommendations.
Management of hypoalbuminemia
Before administering intravenous albumin, the cause of the problem must be found; increasing protein in the diet is a valuable initial step.
Management of fluids and vitamin supplements is frequently used in patients with severe kidney disease and chronic liver disease..
Management of cytostatic extravasation
Stopping the infusion is the logical first step. Conservative management is installed immediately with topical treatments with steroids, anti-inflammatories and dimethyl sulfoxide.
For more serious cases or those that do not improve with the above, surgical cures are indicated, with resection of the affected area with delayed closure when there are signs of granulation.
Management of non-cytostatic drug extravasation
Topical treatment is the choice. Steroid or anti-inflammatory creams, ointments or lotions are very helpful.
Cold dressings are also helpful because they relieve symptoms and decrease inflammation. Catheter function should be checked and replaced if necessary.
Mucocele due to extravasation
Extravasation mucocele is a common lesion in the oral mucosa caused by small lesions of the minor salivary glands..
These damages lead to the accumulation of localized mucous secretion and eventually to the formation of a small lump or cyst which, without being painful, causes certain discomfort..
It differs from the retention mucocele in its etiology. The latter is formed not by damage, but by obstruction of the salivary ducts that drain the minor salivary glands. As its content cannot be released, it encapsulates and generates the cyst.
Some mucoceles disappear spontaneously and do not need treatment. Others may require surgical excision, for which there are different techniques, including minimally invasive procedures and laser surgery..
References
- AMN Healthcare Education Service (2015). Know the Difference: Infiltration vs. Extravasation. Recovered from: rn.com
- Holton, Trudy, and the Committee for Clinical Effectiveness in Nursing (2016). Extravasation Injury Management. The Royal Children's Hospital Melbourne, Retrieved from: rch.org.au
- Wikipedia (last edition 2018). Extravasation (intravenous). Recovered from: en.wikipedia.og
- Alfaro-Rubio, Alberto and collaborators (2006). Extravasation of cytostatic agents: a serious complication of cancer treatment. Dermo-Sifiliographic Actas, 97: 169-176.
- Nallasivam, K. U. and Sudha, B. R. (2015). Oral mucocele: Review of literature and a case report. Journal of Pharmacy & Bioallied Sciences, 2: 731-733.
- Granholm, C. et al. (2009). Oral mucoceles; extravasation cysts and retention cysts. A study of 298 cases. Swedish Dental Journal, 33 (3): 125-130.
- Sinha, Rupam and collaborators (2016). Nonsurgical Management of Oral Mucocele by Intralesional Corticosteroid Therapy. International Journal of Dentistry.
- Wikipedia (last edition 2018). Oral mucocele. Recovered from: en.wikipedia.org


Yet No Comments