
Kwashiorkor Symptoms, Causes, Pathophysiology and Treatment
The term Kwashiorkor It is used to define a severe type of protein-calorie malnutrition in children. It is a common public health problem in poor countries, with a high rate of morbidity and mortality associated with it. It is also known as Childhood Multiple Differential Syndrome or Edematous Malnutrition.
Its name comes from a Ghanaian word, specifically from the Kwa language, which means “the displaced child”. It refers to older children who stop being breastfed when their siblings are born. Their diet is usually replaced by vegetable starches that are high in carbohydrates but very little protein..

Primary malnutrition is generally caused by the concurrence of various environmental and organic factors. However, even with the multiple studies on the subject that have been carried out, its fundamental etiology is not clear. The pathophysiological phenomena that occur during this condition even have intrauterine and pre-oral origins..
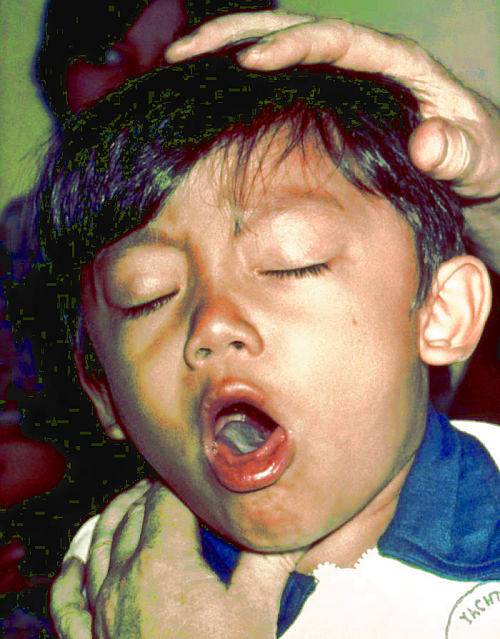
The symptoms of the patient with Kwashiorkor are very dramatic and flowery. They have alterations in many body systems, which makes these children a walking compendium of pediatric pathology. Fortunately, when the appropriate treatment is instituted in time, the response is usually satisfactory and rapid..
Article index
- 1 Symptoms
- 1.1 Skin and mucous membranes
- 1.2 Weight-loss deficit
- 1.3 Metabolic disorders
- 1.4 Gastrointestinal disorders
- 1.5 Blood and cardiovascular disorders
- 1.6 Mental disorders
- 1.7 Immune disorders
- 1.8 Other signs and symptoms
- 2 Causes
- 3 Pathophysiology
- 3.1 Edema
- 3.2 Other pathophysiological events
- 4 Treatment
- 4.1 Initial treatment of the acute phase
- 4.2 Rehabilitation
- 4.3 Follow-up
- 5 References
Symptoms
The signs and symptoms of Kwashiorkor are very diverse in their presentation and severity. Virtually all organs of the economy are affected, some more than others and with a different order of appearance. The most important ones are described below:
Skin and mucous membranes
Among the first changes that children with Kwashiorkor present are changes in skin and hair color.
The skin presents areas of irregular hypo or hyperpigmentation, also becoming thick, scaly and dry. There may be distal acrocyanosis in the hands and feet, associated with peripheral vascular disease.
Hair becomes brittle and thin, dry to the touch and brittle, and patches of alopecia may be scattered on the scalp. One of the most striking characteristics of malnutrition is the progressive discoloration of the hair, from the root to the tip, known as the sign of the flag..
Vitamin deficiencies cause important clinical manifestations in the mucous membranes: the lack of vitamin B causes serious lesions in the mouth and lips; xerophthalmia may be found due to vitamin A deficiency, accompanied by corneal ulcers; and grainy deposits and keratomalacia around natural body openings are not unusual.
Weight-loss deficit
In the Kwashiorkor there is always a compromise in the size and weight of the child. Although these are some of the earliest signs, weight and thinness are occasionally hidden by the characteristic edema of the disease. The height of malnourished patients can be up to 80% below the expected level for their age.
Metabolic disorders
Increased volume - especially in the abdomen, ankles and feet - is a classic sign of Kwashiorkor. This accumulation of fluids begins in the areas of slopes due to gravity and can extend to the face, producing the typical sign of "full moon face". The edema in the lower limbs is symmetrical, painless, cold and leaves pitting on acupressure.

Gastrointestinal disorders
Diarrhea is frequent. Stool may be loose, with food remains that were not digested, or liquid and smelly.
Blood in bowel movements indicates severe intestinal damage. Another common feature in these patients is fatty infiltration of the liver with palpable hepatomegaly.
Blood and cardiovascular disorders
Most cases present with some degree of anemia, which is expected in any deficiency syndrome. The longer the evolution time, the more pronounced the anemia will be.
This results in the presence of compensatory tachycardia and cardiomegaly, as well as abnormal heart rhythms, murmurs on auscultation, and syncope..
Mental disorders
The child's behavior ranges from habitual apathy to occasional irritability. He appears to be absent, with a fixed and lost gaze, often immobile and, paradoxically, inappetent.
Immune disorders
The weakened immune system leads to more and more severe infectious diseases. Opportunistic infections due to atypical germs appear, difficult to treat.
White blood cells are not diminished in quantity, so it is suspected that the immunodeficiency is of humoral rather than cellular origin.
Other signs and symptoms
Cavities are frequent and serious. Early tooth loss is common and dramatic.
Problems with ossification can lead to malformations in the upper and lower limbs, with a tendency towards pathological fractures. The rickety rosary or necklace is a painful find in young people and adults who survived the Kwashiorkor in childhood..
Causes
Kwashiorkor is a severe type of malnutrition. Its most important cause is the lack of energy due to the intake of low-calorie foods.
Currently, it is believed that the lack of macronutrients is more important than the lack of micronutrients in the genesis of the disease, as well as the lack of energy more than the lack of proteins.
However, almost all authors agree that the origin of Kwashiorkor is multifactorial. Some of the elements that play in favor of nutritional deficiencies and the appearance of severe malnutrition include:
- Early and inadequate weaning.
- Increased caloric demand.
- Unbalanced diet.
- Misuse of infant formulas.
- Inadequate feeding times.
- Infections.
- Prematurity.
There are currently two other hypotheses about the appearance of Kwashiorkor: aflatoxin poisoning and the presence of free radicals..
Although both are interesting and innovative, neither has been able to test, at least individually, all the signs and symptoms that characterize the disease.
Pathophysiology
A complex series of pathophysiological events is triggered in individuals with Kwashiorkor. The most important organic mechanisms that contribute to the appearance of the signs and symptoms of the disease are discussed below..
Edema
In the first descriptions of the disease, low serum albumin levels were blamed for edema, but in the 1980s it was assumed that this was not correct because many swollen children retained normal albumin levels. However, the latest studies recover the thesis that hypoalbuminemia is the cause of edema.
Albumin is one of the most important serum proteins thanks to its multiple tasks and, due to its size, it is the main supporter of intravascular oncotic pressure.
As there is a deficiency of albumin, the oncotic pressure is lost within the blood vessels, making their pores more permeable and favoring the extravasation of blood components..
Due to the difference in gradients, the plasma exits from the intravascular space into the interstitium, causing edema and hypovolemia. This phenomenon perpetuates the edematous picture due to the activation of antidiuretic factors and reabsorption of fluids at the renal level, which once again leak into the bloodstream. A vicious circle.
Other pathophysiological events
Certain intrinsic and extrinsic factors can contribute to the development of Kwashiorkor. From an endogenous point of view, a child who eats less food than he requires to satisfy his caloric needs, obtains energy initially from the consumption of body fat, and then by muscle proteolysis.
Neoglycogenesis in the liver is increased, there is a loss of subcutaneous fat and muscle fatigue. This contributes to weight and height deficiencies, as well as the development of musculoskeletal and behavioral disorders. In addition, liver involvement impairs the production of other substances necessary for gastrointestinal function.
This scenario leads to various metabolic changes necessary to maintain the functioning of the body.
When the diet does not cover protein needs and carbohydrate consumption is high, it leads to edema, lack of pigmentation of the skin and integuments, and finally anemia and immunodeficiency.
Treatment
The management of the severely malnourished patient must be multidisciplinary and continuous. If done correctly, the success rate is overwhelming. Children respond very well when therapy is started on time and by following all steps properly.
The WHO proposes a management in three phases. The first, and most complex, must be done with the hospitalized patient and following a series of very precise steps. The other two are carried out on an outpatient basis. The intervention is applied as follows:
Initial treatment of the acute phase
It corresponds to the first days of treatment, which usually represent the most critical in the patient's health. In its application, 10 fundamental steps must be followed:
Treat and prevent hypoglycemia
Any blood glucose value below 54 mg / dL should be treated with highly concentrated dextrose solutions (minimum 10%). Upon reaching glycemic levels above 70 mg / dL, maintenance glucose hydrations are indicated.
Treat and prevent hypothermia
If the patient has temperatures below 35 ºC, feeding and hydration should be started immediately. It should be covered completely and use thermal blankets if necessary. Avoid bags or bottles with hot water, as they can cause burns.
Treat and prevent dehydration
Special solutions should be used for malnourished children or lactated ringer if the first is not available. Adapt management according to local oral or parenteral rehydration protocols.
Correct electrolyte imbalances
One must be very cautious with serum sodium because correcting it in excess can be lethal. Potassium and magnesium are the other electrolytes that are most altered and their correction can be done orally or intravenously. Normal values can take up to two weeks to reach.
Treat and prevent infections
Active infections must be managed with broad-spectrum antibiotics. Always remember that malnourished children may not have fever or alterations in laboratory tests even with serious infectious diseases.
Many authors recommend the use of metronidazole to eradicate gastrointestinal bacteria and parasites, and promote the recovery of the local mucosa. Once the child is in better condition, the usual vaccination schedule should be started or completed..
Correct micronutrient deficiencies
Vitamin and mineral supplements should be given with the diet. Iron therapy should be started when the child is eating normally and has gained weight at the expense of fat and muscle, not due to edema.
Start feeding wisely
It is vitally important to start feeding the child as soon as he or she enters the care center. The amount of protein and calories necessary for its normal development must be strictly adhered to. Oral feeding should be encouraged with small but frequent intakes.

Achieve growth recovery
Once the child tolerates feeding adequately, a weight recovery regimen should be started. This usually takes a week and continues in the rehabilitation and follow-up stage..
Sensory stimulation and emotional support
In these patients there will always be a compromise of mental, behavioral and affective development. They will need a happy and cordial environment, with people who show them care and affection, involving the parents if they are present.
Prepare for follow-up after recovery
When about 90% of normal body weight has already been recovered, you are in the presence of a physically recovered child. Size can take longer to improve and can sometimes be unrecoverable. Feeding and emotional support should continue at home.
Rehabilitation
This phase is primarily nutritional and takes place at home or wherever the child is going to stay. Affective and emotional support should be increased, with the participation of the family and facilitators.
Refeeding syndrome is a possibility at this stage, so abrupt food increases should be avoided..
Tracing
After discharge, permanent surveillance of the child and his environment must be maintained. Relapses are frequent and very traumatic. The adequate physical, intellectual, emotional and mental development of the child must be guaranteed, progressively, until normality is achieved.
References
- Borno, Sonia and Noguera, Dalmatia (2009). Calorie-Protein Malnutrition. Pediatric Nutrition, Venezuelan Society of Childcare and Pediatrics, chapter 9, 225-240.
- Ashworth, Ann; Khanum, Sultana; Jackson, Alan and Schofield, Claire (2004). Guidelines for the inpatient treatment of severely malnourished children. World Health Organization, retrieved from: who.int
- World Health Organization (1999). Management of severe malnutrition. Recovered from: apps.who.int
- Healthline Editorial Team (2017). What is Kwashiorkor? Recovered from: healthline.com
- United Nations Food Organization (2000). Protein-energy malnutrition. Malnutrition Disorders, part III, chapter 12, retrieved from: fao.org
- Coulthard, Malcolm G. (2015). Oedema in kwashiorkor is caused by hypoalbuminaemia. Paediatrics and International Child Health, 35 (2): 83-89.
- Kismul, Hallgeir; Van den Broeck, Jan and Markussen Lunde, Torleif (2014). Diet and kwashiorkor: a prospective study from rural DR Congo. Peer-Reviewed & Open Access, 2: 350.
- James, W P (1977). Kwashiorkor and marasmus: old concepts and new developments. Proceedings of the Royal Society of Medicine, 70 (9): 611-615.
- Wikipedia (last edition 2018). Kwashiorkor. Recovered from: en.wikipedia.org

Yet No Comments