
Transcranial magnetic stimulation what it is for and types

The transcranial magnetic stimulation is a non-invasive brain stimulation technique whose use has experienced a great increase in recent years, not only in the field of research, but also in the clinical area with rehabilitation and therapeutic exploration.
This type of brain stimulation techniques allow modulating brain activity without the need to penetrate through the cranial vault to directly reach the brain..
Within the brain study techniques, we can find various techniques, however the most used are transcranial direct current stimulation (tDCS) and, to a greater extent, transcranial magnetic stimulation, (Vicario et al., 2013).
Article index
- 1 What is transcranial magnetic stimulation used for??
- 2 Concept of brain plasticity
- 3 What is transcranial magnetic stimulation?
- 3.1 Principles of transcranial magnetic stimulation
- 4 Types of transcranial magnetic stimulation
- 4.1 Transcranial magnetic stimulation, electroencephalography (EEG) and magnetic resonance imaging (MRI) techniques
- 5 Brain stimulation and pathology
- 5.1 Vascular diseases
- 5.2 Epilepsy
- 5.3 ADHD
- 5.4 TEA
- 5.5 depression
- 5.6 Schizophrenia
- 6 Limitations
- 7 Bibliography
What is transcranial magnetic stimulation used for??
Due to their neuromodulation capacity, these techniques can be used for the exploration and modulation of different brain functions: motor skills, visual perception, memory, language or mood, with the aim of improving performance (Pascual Leone et al., 2011 ).
In healthy adults, they have generally been used to monitor cortical excitability and as neuromodulation techniques to induce brain plasticity. However, the use of these techniques in the pediatric population is limited to the treatment of some diseases, to rehabilitate damaged functions (Pascual leone et al., 2011).
Currently, its use has expanded to the area of psychiatry, neurology and even rehabilitation since numerous neurological and psychiatric diseases in childhood and adolescence present alterations in brain plasticity (Rubio-Morell et al., 2011).
Among the cognitive functions that seem to improve are those caused by Parkinson's disease, motor control after a stroke, aphasia, epilepsy and depression, among others (Vicario et al., 2013).
Brain plasticity concept
Brain plasticity represents an intrinsic property of the central nervous system. It is essential for the establishment and maintenance of brain circuits, through the modification of structures and functions in response to environmental demands (Pascual Leone et al., 2011)
The brain is a dynamic organ that uses mechanisms such as potentiation, weakening, pruning, addition of synaptic connections or neurogenesis to adapt its architecture and circuitry, allowing the acquisition of new skills or adaptation after injury. It is an essential mechanism for the ability to learn, remember, reorganize and recover from brain damage (Rubio-Morell et al., 2011).
However, the existence of atypical plasticity mechanisms may imply the development of pathological symptoms. Excess plasticity or hyperplasticity will imply that brain structures are unstable and that functional systems essential for optimal cognitive functioning may be affected..
On the other hand, the deficit of plasticity or hypoplasticitycan be detrimental to the adaptation of our behavioral repertoire to the environment, that is, that we are unable to adjust to changing environmental demands (Pascual leone et al., 2011)
An updated view of the etiology of psychiatric disorders relates these alterations to disorders in specific brain circuits, rather than as focal structural alterations or neurotransmission (Rubio-Morell, et al., 2011).
Therefore, brain stimulation methods, ultimately, can allow interventions based on the modulation of plasticity, due to their ability to induce long-term changes and thus optimize the situation of each individual (Pascual leone, et al., 2011)
What is transcranial magnetic stimulation?
Transcranial magnetic stimulation is a focal, painless and safe procedure (article Rubio-Morell, et al). Due to its neuromodulation capacity, it is capable of producing transitory changes at the level of brain plasticity through the modification of cortical excitability states (Rubio-Morell et al., 2011).
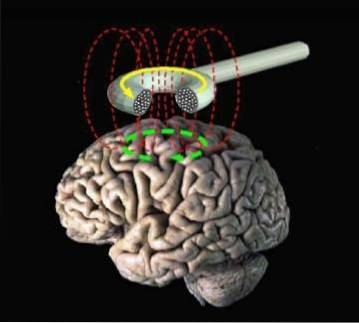
It is a procedure that is used to create electrical currents in discrete regions, through the application of fast and changing electromagnetic pulses, on the scalp of the individual with a copper coil connects.
The electromagnetic field penetrates through the skin and skull and reaches the cerebral cortex to influence changes at the level of neuronal excitability.
The devices used in the application of transcranial magnetic stimulation and magnetic fields are varied. In general, stimulators use stimulation coils of different shapes and sizes that are used on the surface of the scalp.
The coils are constructed from copper wire that is insulated with a plastic mold. The most used coil forms are the circular and the eight-shaped coil (manual manolo).
Principles of transcranial magnetic stimulation
This technique is based on the principle of electromagnetic induction of M. Faraday, from which a magnetic field that, depending on the time, presents a rapid oscillation, will be able to induce a small intracranial electric current in the neurons of the underlying cerebral cortex..
The electrical current that is used, it is a magnetic field that is applied to the scalp in a specific region, induces an electrical current in the cerebral cortex that is parallel and in the opposite direction to the one received..
When the electrical stimulation current is focused on the motor cortex, and an optimal intensity is used, a motor response or motor evoked potential will be recorded (Rubio-Morell et al., 2011).
Types of transcranial magnetic stimulation
One type of transcranial magnetic stimulation is repetitive (rTMS), which consists of the application of several electromagnetic pulses in rapid succession. Depending on the stimulation frequency at which these pulses are emitted, it will induce different changes.
- High frequency stimulation: When stimulation uses more than 5 electromagnetic pulses per second, excitability of the stimulated pathway will increase.
- Low frequency pacing: When stimulation uses less than one pulse per second, the excitability of the stimulated pathway will decrease.
When this protocol is applied, it can induce robust and consistent responses in subjects and lead to potentiation or depression of amplitudes of motor evoked potentials depending on stimulation parameters..
An rTMS protocol, known as Theta Burst Stimulation (TBS), mimics the paradigms used to induce long-term potentiation (PLP) and long-term depression (DLP) in animal models..
When applied continuously (CTBS), the stimulation will evoke potentials that will show a marked decrease in amplitude. On the other hand, when applied intermittently (ITBS), potentials with a greater amplitude will be identified (Pascual leone et al., 2011).
Transcranial magnetic stimulation, electroencephalography (EEG) and magnetic resonance imaging (MRI) techniques
Real-time integration of transcranial magnetic stimulation with EEG can provide information on local cortical response and distributed network dynamics in healthy and diseased subjects..
The use of transcranial magnetic stimulation and MRI as an outcome measure allows the implementation of a variety of sophisticated techniques to identify and characterize the connectivity networks between different brain regions..
Thus, several studies have shown that the architecture of brain networks varies during normal aging and can be abnormal in patients with a variety of neuropsychiatric conditions such as schizophrenia, depression, epilepsy, autism spectrum disorder or deficit disorder. attention and hyperactivity.
Brain stimulation and pathology
One of the main applications of transcranial magnetic stimulation is its application to the improvement of performance or symptoms caused by different developmental disorders, neuropsychiatric disorders or acquired brain damage can affect the functioning of brain plasticity.
Vascular diseases
The pathology of vascular diseases is related to a hemispheric imbalance, in which the activity of the damaged hemisphere is compensated by an increase in the activity of the contralateral homologous area..
Different studies with the application of the rTMS protocol show its potential for the rehabilitation of motor symptoms: increase of grip strength or reduction of spasticity.
Epilepsy
Epilepsy is a pathology that involves the suffering of seizures due to a hyper-excitability of the cerebral cortex.
A varied number of studies with childhood patients with focal-type epilepsy have shown a significant reduction in the frequency and duration of epileptic seizures. However, this conclusion is not generalizable since there is not a systematic reduction in all participants..
ADHD
Attention deficit hyperactivity disorder is associated with hypo-activation of different pathways, specifically in the dorsolateral prefrontal cortex.
The study by Weaver et al. Shows a global clinical improvement and the results of the evaluation scales in individuals with ADHD after the application of different transcranial magnetic stimulation protocols..
TORCH
In the case of autism spectrum disorder, an increase in general gamma activity is described, which may be related to the different attentional, linguistic or working memory alterations that these individuals present.
Different investigations suggest benefits of the therapeutic use of transcranial magnetic stimulation in children with ASD. Participants show a significant improvement in gamma activity, improvement in behavioral parameters, attentional improvements, and even an increase in scores related to vocabulary acquisition..
However, due to the small number of studies and the use of a variety of stimulation protocols, it has not been possible to identify an optimal protocol for its therapeutic use..
Depression
Depression in children and adolescents seems to be associated with an imbalance in the activation of different areas such as the dorsolateral prefrontal cortex and limbic regions. Specifically, there is hypoactivation in the left regions, while in the right, there is hyperactivation of these structures.
The available studies suggest the existence of clinical effects of the use of rTMS protocols: reduction of symptoms, improvement and even clinical remission.
Schizophrenia
In the case of schizophrenia, on the one hand, an increase in excitability of the left temporo-parietal cortex has been identified, associated with positive symptoms and, on the other hand, a decrease in left prefrontal excitability, related to negative symptoms.
The results on the effects of transcranial magnetic stimulation in the pediatric population show signs of a reduction in positive symptoms, hallucinations.
Limitations
Overall, these studies show preliminary evidence on the potential of brain stimulation techniques. However, different limitations have been identified, among which is the scarce use of stimulation techniques, generally associated with serious pathologies or in which the pharmacological treatment does not present a significant effect..
On the other hand, the heterogeneity of the results and the different methodologies used make it difficult to identify the optimal stimulation protocols.
Future research should deepen our knowledge of the physiological and clinical effects of transcranial magnetic stimulation..
Bibliography
- Pascual-Leone, A., Freitas, C., Oberman, L., Horvath, J., Halko, M., Eldaief, M., Rotenberg, A. (2011). Characterizing Brain Cortical Plasticity and Network Dynamics Across the Age-Span in Health and Disease with TMS-EEG and TMS-fMRI. Brain Topogr.(24), 302-315.
- Rubio-Morell, B., Rotenberg, A., Hernández-Expósito, S., & Pascual-Leone, Á. (2011). Use of non-invasive brain stimulation in childhood psychiatric disorders: new opportunities and diagnostic and therapeutic challenges. Rev Neurol, 53(4), 209-225.
- Tornos Muñoz, J., Ramos Estébañez, C., Valero-Cabré, A., Camprodón Giménez, J., & Pascual-Leone Pascual, A. (2008). Transcranial Magnetic Stimulation. In F. Maestú Unturbe, M. Rios Lago, & R. Cabestro Alonso, Neuroimaging. Cognitive techniques and processes (pp. 213-235). Elsevier.
- Vicario, C., & Nitsche, M. (2013). Non-invasive brain stimulation for the treatment of brain diseases in childhood and adolescence: state of the art, current limits and future challenges. Frontiers in systems neurscience, 7(94).
- Image source.



Yet No Comments