
Chronic stress symptoms, causes, risk factors, treatments

The chronic stress it is a type of adjustment disorder characterized by an unhealthy emotional and behavioral reaction to an identifiable and prolonged stress situation. It differs from anxiety in that in this the stressful stimulus is not identifiable.
Stress is an adaptive response of our body to an excessive demand from the environment or to a situation with a high emotional charge. Stressful situations can be both negative and positive, for example they can cause us the same stress to show up for an important exam and get married.

This ability allows us to prepare to respond to stressful stimuli. To do this, you must first become aware of the situation. If we identify the stimulus as stressful, the neuroendocrine system will be activated and a neurophysiological response will be emitted, characterized by a rise in activation levels.
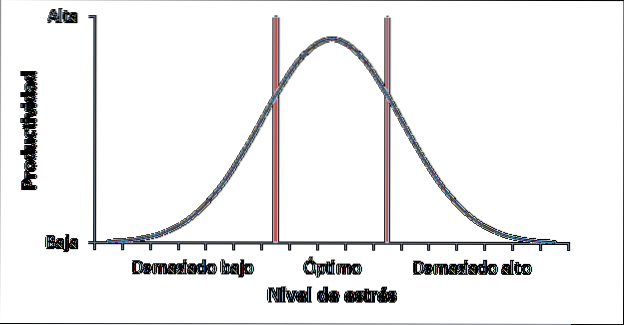
When intermediate stress levels are reached, our performance in the face of the stressful situation will be optimal, but if the stressful situation continues to occur for a long time, our neuroendocrine system is depleted, stress is no longer adaptive and chronic stress appears (see Figure 1).
The levels of stress necessary to reach the optimum level and to reach chronic stress depend on many variables (context, personality, type of stimulus); therefore it varies from person to person.
Article index
- 1 Characteristics of chronic stress
- 2 Symptoms of chronic stress
- 3 Course and prognosis
- 4 Who can suffer from chronic stress?
- 5 Risk or protective factors
- 5.1 Individual
- 5.2 Social
- 6 Treatment
- 6.1 Psychotherapeutic treatment
- 7 References
Characteristics of chronic stress
The emotional and behavioral reaction to chronic stress must occur within 3 months after the stressful situation has occurred and must be of great intensity.
This disorder includes the following symptoms (according to DSM-V):
- Greater discomfort than expected in response to the stressful stimulus.
- A significant deterioration in social and work (or academic) activity.
To speak of chronic stress, the above symptoms must persist for more than 6 months. It is important to clarify that these symptoms should not respond to a grieving reaction, since in that case it would be a normal response, not a maladaptive one..
Chronic stress symptoms
People who suffer from chronic stress may experience the following symptoms:
- Depressed mood, sadness.
- Trouble breathing.
- Chest pain.
- Anxiety or worry.
- Feeling of inability to deal with problems.
- Difficulty performing your daily routines.
- Feeling unable to plan ahead.
Course and prognosis
Most symptoms diminish and often disappear as time passes and stressors are eliminated, without the need for any type of treatment..
However, when stress becomes chronic it is more difficult for this to occur, since it can facilitate the appearance of other disorders such as depression or anxiety, or even promote the use of psychoactive substances.
Who can suffer from chronic stress?
It is estimated that between 5-20% of the population that has been assisted by psychological problems suffer from an adjustment disorder (which includes chronic stress). In children and adolescents this percentage increases, reaching between 25-60%.
Chronic stress can be suffered at any age, although it is especially common in children and adolescents, and affects women and men indifferently.
Cases of chronic stress occur throughout the world, but the way in which these cases manifest themselves and the way of studying them varies markedly depending on the culture.
Furthermore, cases of chronic stress are more numerous in disadvantaged cultures or in developing countries. Likewise, they tend to be more frequent in populations with low socioeconomic levels..
Risk or protective factors
There are many factors or variables that can increase or decrease the probability of suffering from an adjustment disorder, although no variable is known that by itself determines the appearance of this disorder..
The variables can be:
Individuals
The individual variables that can influence the development of an adjustment disorder are those that influence the way in which the person perceives and copes (coping) with stressful situations. These variables include:
- Genetic determinants. Certain genotypes can make the individual have a greater predisposition or vulnerability to stressful situations.
- Social skills. People with better social skills will be able to seek the necessary support in their environment.
- The intelligence. Smarter people will develop more effective strategies to cope with the stressful situation.
- Cognitive flexibility. Flexible individuals will adapt better to situations and will not perceive them as stressful.
Social
The social environment is very important both as a risk factor and as a protector, since it can be another tool to cope with stress but it can also lead to the appearance of certain stressors (divorce, abuse, bullying). The main social variables are:
- The family: it can be a strong protective barrier against stress, if there is a good family relationship, but it can also be stressful if it is an unstructured family or with particularly authoritarian educational styles. It should be borne in mind that it is not convenient either to share all the stress with the family since this can destroy the family nucleus.
- The peer group: friends (or colleagues) in adolescence and the partner in adulthood are very influential factors during our lives. As with the family, they can be both risk and protective factors. But, unlike what happened with the family, we can choose the people around us, therefore it is important to recognize when they are constituting risk factors and eliminate them from our lives if necessary..
Treatment
The design of the treatment will depend on multiple factors, among which it is worth highlighting:
- the age of the person.
- Your general condition and medical history.
- The specific symptoms you suffer from.
- If you have any subtype of the disorder.
- The tolerance or susceptibility of the person to certain medications or therapies.
It is recommended to use multimodal holistic treatments that include the important areas of the patient's life, for example, psychotherapy, family therapy, behavior modification, cognitive restructuring and group therapy could be combined.
All treatments pursue the same objectives:
- Relieve symptoms that are already occurring, for which relaxation techniques can be very helpful.
- Teach the person and offer support to handle the current stressful situation, and possible future situations as well as possible.
- Reinforce and, if necessary, restructure the social environment. For this, new ties must be created and existing ones reinforced, starting with forming a healthy psychologist-patient relationship..
- Identify the individual factors that may favor or hinder the development of the disorder and adherence to treatment.
- Follow maintenance to assess patient progression.
Regarding the nature of the treatment, psychological or psychopharmacological, it is recommended to start with psychotherapy and start with psychoactive drugs only if necessary, but always continuing with psychotherapy.
Psychotherapeutic treatment
There are very diverse treatments but we will focus on cognitive-behavioral and systemic therapy as they are the most used.
Cognitive behavioral therapy
This approach is aimed at teaching the patient to develop their own tools to solve problems, to improve communication and to manage impulses, anger and stress..
The intervention focuses on modifying thoughts and behaviors in order to improve coping strategies. This approach includes a wide variety of techniques, such as biofeedback, problem solving, cognitive restructuring, relaxation techniques, among others..
Systemic therapy
Of the systemic therapies the most common are:
- Family therapy. This therapy is aimed at modifying the necessary aspects in the family to make it a protective factor. For this, knowledge of the patient's problem, communication and interaction between family members and mutual support are promoted..
- Group therapy. This type of therapy is usually done when the patient is getting better. It can be very useful but care must be taken, as it can cause the patient not to identify his responsibility for the problem and therefore not work to recover because he believes that he does not depend on himself.
Psychopharmacological treatment
Psychotropic drugs are only indicated in cases that are particularly resistant to psychotherapy and in severe cases (such as the subtypes of adjustment disorder with anxiety or depression), but they should always be accompanied by psychotherapy.
It is important to take the drug only when the doctor prescribes it and in the doses indicated by the doctor, since the choice of the psychoactive drug to take depends on multiple factors. For example, not all antidepressants have the same effects, and it can be very dangerous to take the wrong psychoactive drug (or in the wrong dose) and can even cause other disorders.
In the case of chronic stress, anxiolytics or antidepressants are usually pre-registered depending on the patient's symptoms. Only if anxiety is very intense, low-dose antipsychotics can be indicated. In specific cases where there is significant inhibition or isolation, psychostimulants (for example amphetamines) can also be pre-registered.
References
- Batlle Vila, S. (2007-2009). Adjustment Disorders. Master in Paidopsychiatry. Barcelona: Autonomous University of Barcelona.
- Carlson, Neil (2013). Physiology of Behavior. Pearson. pp. 602-606. ISBN 9780205239399.
- González de Rivera and Revuelta, J. (2000). ADAPTIVE AND STRESS DISORDERS. Virtual Congress of Psychiatry. Retrieved on March 2, 2016, from psiquiatria.com.
- Holmes, T., & Rahe, R. (1967). The social readjustment rating scale. J. Psychoson. Beef., 213-218.
- MedlinePlus. (October 3, 2014). Medical encyclopedia. Obtained from Adjustment Disorder.
- Perales, A., Rivera, F., & Valdivia, Ó. (1998). Adjustment disorders. In H. Rotondo, Psychiatry Manual. Lima: UNMSM. Obtained from sisbib.unmsm.edu.pe.
- psychomed. (s.f.). DSM-IV. Obtained from Adaptive Disorders psicomed.net.
- Rodríguez Testal, J. F., & Benítez Hernández, M. M. (s.f.). Adaptive Disorders. Clinical Psychopathology. Seville: University of Seville.


Yet No Comments