
Blood smear characteristics, types, techniques and histology

The Blood smear It is a peripheral blood smear that is used to analyze the components present in the blood circulation. The observation of a blood smear provides hematological data that are very useful for the diagnosis and follow-up of many pathologies..
The blood smear allows to quantify the number of the different types of white blood cells (leukocyte formula), as well as allows the analysis of the morphology and shape of erythrocytes, leukocytes and platelets.

It can detect abnormalities in the number of cells, such as: leukocytosis or leukopenias, lymphocytosis or lymphopenia, neutrophilia or neutropenia, thrombocytosis or thrombocytopenias and eosinophilia. Cell shape and size abnormalities may also be seen.
Additionally, it is possible to detect various types of anemias, leukemias, and bacterial or blood parasite infections..
For this, there are various types of smears that are performed depending on the purpose of the study. There are thin smears and thick smears. These smears differ in the execution technique and the purpose of the study..
Those with fine drops are used as an adjunct to complete hematology. This provides data on the leukocyte formula, in addition to the analysis of the shape and morphology of the three cell series that make up the blood: red series, white series and platelets. Although they also serve as a complement to the study of thick blood film.
Thick blood film is used for the diagnosis of diseases caused by hemoparasites, such as malaria or malaria, toxoplasmosis, leishmaniasis, Chagas disease, babesiosis and microfilariasis.
Article index
- 1 Characteristics of a blood smear
- 2 Types of blood smear
- 3 Techniques for taking blood samples
- 4 Techniques for the preparation of the blood smear
- 4.1 -Slides smears
- 4.2 -Frosting on coverslips
- 4.3 -With automated equipment
- 5 Thick smear technique
- 6 Staining of smears
- 6.1 Giemsa stain
- 6.2 Wright's stain
- 7 Types of defective smears
- 7.1 Smears with areas of different thicknesses (thin and thick interspersed)
- 7.2 Smears with very short smears
- 7.3 Smear with a raked area towards the end of the smear
- 7.4 Smears with formation of vacuoles or clear rounded or elliptical areas
- 7.5 Very thick or very thin smears
- 8 Histology
- 8.1 -Erythrocytes or red blood cells
- 8.2 -White blood cells or leukocytes
- 8.3 -Platelets
- 9 Pathological elements
- 9.1 Blood parasites
- 9.2 Bacteria
- 9.3 Immature cells
- 10 References
Characteristics of a blood smear
A good blood smear must meet certain characteristics. Among them we can mention:
-The sample must meet the minimum quality requirements to be representative.
-The sampling must be well executed.
-Timely execution of the smear.
-If performed with venous blood, use an anticoagulant that does not deform the cells and mix the tube before taking the smear.
-If it is done with capillary blood, discard the first drop.
-The spread must be homogeneous. This ensures that the cells are evenly distributed and that a good analysis of the blood cells, in terms of shape and number, can be done..
-The sides of the smear should be smooth from start to finish.
-The smear should respect a margin of 1 to 2 mm to the sides of the slide.
-The smear layer should gradually decrease in thickness from the beginning to the end (fine-drop smear by the slide method).
-Must be properly labeled to avoid sample confusion.
-Fix and stain appropriately for clear observation of blood elements.
-Allow the smear to dry very well before mounting the preparation under the microscope. Placing oil immersion on a wet smear will cause the formation of micelles that prevent the cells from being seen..
Types of blood smear
Peripheral blood smears can be classified into thin smear and thick smear. Those with a thin layer are used for the study of the leukocyte formula and morphological observation of blood cells. You can also see extracellular bacteria such as borrelia and intracellular hemoparasites, such as plasmodium, among others..
In the fine blob, the species of the parasite can be identified, therefore, it is a more specific technique than the thick blob, but the thick blob is more sensitive, since it is a concentration technique used for the exhaustive search for extracellular hemoparasites..
There are two types of fine-drop smears: those performed on slides and those performed on coverslips. The thick smears are performed on slides.
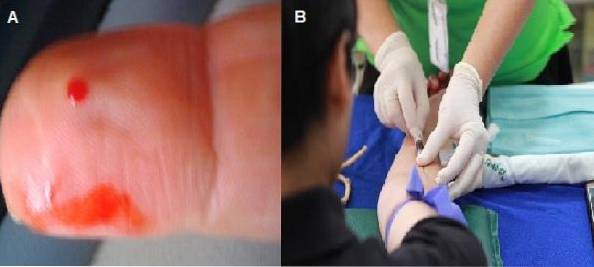
Techniques for taking blood samples
Blood smears can be made from a capillary puncture or a venous sample taken with anticoagulant. If it is done from blood with anticoagulant, the smear can be prepared up to 2 hours after taking the sample..
Caution should be taken to use anticoagulants that do not deform blood cells. The best option is EDTA. On the contrary, the use of anticoagulants such as trisodium citrate should be avoided..
If the sample is taken by capillary puncture, the smear should be extended immediately, before the blood clots.
The first drop should be discarded, allowing the next drop to escape spontaneously to avoid dilution of the sample with the tissue fluid. It is the most recommended technique for the observation of cell morphology, since the blood does not have any additives.
For the observation of hemoparasites, Solari et al. Concluded in their research that both techniques (venipuncture and capillary) are equally efficient..
Techniques for the preparation of the blood smear
The blood smear can be performed manually on microscope slides or on coverslip or slide. It is also possible through automated equipment.
-Smear on slides
It is the technique preferred by most laboratories due to its easy handling..
Using a Pasteur pipette, place a not very thick or very fine drop of blood in the center of one end of a clean microscope slide..
The smear is made with the help of another slide with a ground end. The ground glass slide is placed perpendicular to the opposite end of the drop..
It leans to an angle between 30 - 45 ° and slides towards the drop; When touched, it expands linearly over the edge of the ground slide and with a constant and defined movement the sheet returns; before reaching the end the slide is lifted.
In this way, a homogeneous layer is spread over the surface of the receiving slide..
The smear is allowed to dry. It is then fixed and stained with the preferred stain. Allow to dry well before viewing under the microscope. A drop of oil is placed on the face that presents the smear and is observed under a light microscope.
Parts of the smear made on slides
In this type of smear, three defined areas can be distinguished: the head, the body and the tail. The head corresponds to the area where the smear starts, it is the thickest area and it is not good to observe.
The body is the central or intermediate part of the smear, it is the best area to observe under the microscope, since there the cells are uniformly distributed and their morphology is preserved.
The tail corresponds to the final part of the smear; here the distribution is no longer uniform and the morphology of the erythrocytes tends to be lost.
Quality control in the slide technique
In this technique it plays a fundamental role:
-Cleaning and degreasing of the microscope slide: ensures good slide of the specimen.
-The size of the drop: with very large drops a thicker and longer smear will be obtained, with a very small drop the spread will be shorter and extremely fine.
-The speed applied in the extension: the lower the speed the smear will be thinner, the higher the speed it will be thicker.
-The angle of execution: the smaller the angle the finer the smear, the higher the angle the thicker.
-Smear on coverslip
It is not widely used because it is cumbersome to handle fragile coverslips, however it offers great advantages, since a better distribution of cells is obtained throughout the smear..
A not very thick or very fine drop is placed in the center of a coverslip. Immediately another coverslip is placed on top of it in such a way that the tips of both coverslips protrude, forming a star.
The drop will spontaneously spread over the surface of both coverslips. At the end of the extension, each lamella slides to the opposite side of each other (one to the right and the other to the left) quickly.
The technique provides two smears instead of one.
They are placed to dry with the spread side up. Once dry, it is fixed and stained with the technique of choice. Let it dry. A drop of immersion oil is placed on a slide, the smear is placed with the smear side down, and viewed under a microscope..
Quality control in the coverslip technique
To obtain a good smear for this technique it is important to:
-Cleaning of the coverslips (helps the good glide of the sample).
-The size of the drop (influences the thickness of the smear).
-The speed with which the coverslips are separated (influences the homogeneity of the smear).
-With automated equipment
They can be done through any of these equipment: Spinner and Autoslide.
The Spinner consists of placing a slide with a drop of blood on a special centrifugation plate. The sample is centrifuged at high speeds; in this way a homogeneous and fine smear of the sample is formed. Disadvantage of the possibility of hemolysis of the sample.
The Autoslide is an instrument that mechanically performs the movements for the execution of the smear on slides. You can also fix and stain the smear. It can even be adapted to some automatic hematology counters.
Thick smear technique
To search for haemoparasites, it is recommended to perform two smears: one with a fine drop and one with a thick drop..
Perform a capillary puncture, clean the first drop. Place a fine drop on a slide and smear as previously explained. For the thick bead, place a large bead on another slide and spread into a 1.55mm square. Let the two smears dry.
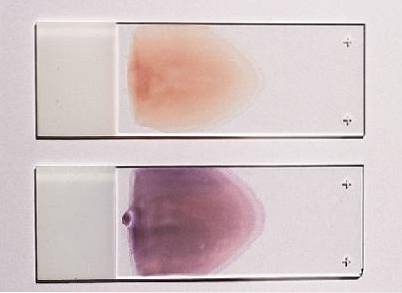
Smear staining
For those with fine drops, Giemsa or Wright stains, among others, can be used. Giemsa or May-Grunwald Giemsa stain is recommended for thick smears.
Giemsa stain
The smear is fixed for 3 minutes with methanol, drained and allowed to dry again. The smear is then covered with Giemsa stain for 10-15 minutes. It is washed with distilled water and allowed to dry. To observe under the microscope a drop of immersion oil is placed.
Wright's stain
The smear is covered with Wright's stain for 5 minutes. Discard and place the buffer solution at pH 6.8 for 6 minutes. Blow the preparation to homogenize. Wash with distilled water and allow to dry. Observe under the microscope.
Defective smear types
Occurs in trainees of the fine drop technique with slides.
Smear with areas of different thicknesses (thin and thick interspersed)
It is because the movement executed was not constant during the spread, making stops and restarts.
Very short smear smear
They have 2 causes: one is due to the fact that the ground slide has been lifted before reaching the other end of the slide. In this case it is extremely thick and short.
On the other hand, if the smear is short but thin, it is because the size of the drop was very small..
Smear with a raked area towards the end of the smear
It has several causes: one is that the ground edge is defective, that the pressure exerted on the receiving slide is increased at the time of spreading or that the ground edge of the slide is worn.
Smear with formation of vacuoles or clear rounded or elliptical areas
They are due to the use of greasy smears (poorly washed and degreased).
Very thick or very thin smears
Drops that are too large will produce very thick smears from start to finish and very small drops will produce very fine smears.
Histology
Blood cells can be seen in a blood smear. Among them are:
-Erythrocytes or red blood cells
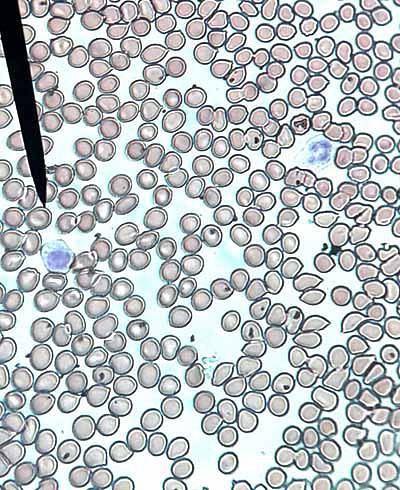
The number of erythrocytes or red blood cells is approximately 5 x 106 mm3 in man and 4.5 x 106 in women. Red blood cells are shaped like biconcave discs, with a central physiological pallor. Can be seen separately (normal) or stacking in rouleaux (abnormal).
Smears also show poikilocytosis (red cells of various shapes), anisocytosis (red cells of various sizes), anisopoikilocytosis (various shapes and sizes), anisochromia (different colors), erythroblasts (immature red cells), microcytosis (smaller red cells) ) and macrocytes (larger erythrocytes).
When they present a deficiency in the amount of hemoglobin and the central pallor increases, it is said that there is hypochromia. When a normal red series is observed, it will be reported as normocytic and normochromic..
-White blood cells or leukocytes
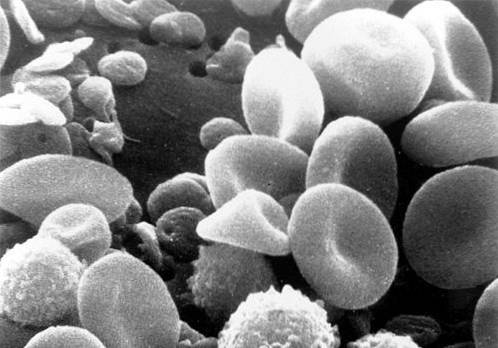
The normal quantity ranges from 5,000 to 10,000 mm3. They are altered in infectious processes, in allergies and in leukemia. In the blood smear, several types can be distinguished, which are explained below.
Segmented neutrophils
They represent 55-65% of the total leukocytes. They measure between 10-15 μm. They have a segmented or lobed nucleus that adopts various morphologies, hence it is called polymorphonuclear.
They have abundant neutrophilic granules in their cytoplasm and some azurophils. Increase in bacterial infections (neutrophilia), decrease in viral infections (neutropenia).
Morphological abnormalities can be observed such as pleokaryocytosis (hyper-segmented nuclei), arch (immature cells) or macropolicites (oval-shaped and large).
Other alterations:
-Toxic granulations
-Pseudo Pelger neutrophils (nucleus are unlobed or bilobed).
-Döhle bodies: dark blue cytoplasmic inclusions.
-Increased cytoplasmic basophilia.
-Intracytoplasmic vacuoles.
-Cellular pyknosis (loss of internuclear bridges).
Segmented eosinophils
They represent 1-3% of the total white blood cells. They measure 9-10 μm. They are characterized by the presence of abundant acidophilic cytoplasmic granules and few azurophiles. Its nucleus has two lobulations. Their number increases in allergies and diseases of parasitic origin.
Segmented basophils
They are extremely rare, representing 0-1% of leukocytes. They measure 10-12μm. The nucleus is usually irregular in borders and may be bilobed, but it is not observed due to the large number of basophilic coarse granulations in its cytoplasm. Very rarely basophilia may be seen.
Lymphocytes
They are small cells with basophilic cytoplasm, with a well-defined, round nucleus, with condensed chromatin. The nucleus encompasses almost the entire cell. They represent 26-40% of blood leukocytes. They increase in viral infections (lymphocytosis). Reactive lymphocytes can be seen.
Monocytes
Cells larger than lymphocytes, with larger cytoplasm and looser chromatin oval nuclei. They measure 9-12μm. The cytoplasm is abundant and usually appears pale grayish-blue with standard staining techniques. Vacuolated monocytes and monocytosis can be observed among the alterations..
-Platelets
They measure between 1.5-3 μm. Its shape is round or oval. The normal value ranges from 150,000 to 350,000 platelets / mm3. They can decrease in some viral infections. They have no nucleus and are colored purple. Abnormalities may be seen in this series, such as macro or micro platelets, thrombocytosis or thrombocytopenia, and platelet fragments.
Pathological elements
Hematic parasites
Hemoparasites, such as the causative agent of malaria or malaria (parasites of the genus Plasmodium), may be seen in blood smears. For this reason, it is important that the smear be analyzed manually, since automated equipment overlooks this finding..
Bacteria
In pathologies such as relapsing fever or Lyme disease, its causative agent can be observed. In this case it corresponds to the spirochetes Borrelia recurrenti Yet the Borrelia burgdorferi in the blood smear.
Immature cells
Severe cases are observed in leukemias, leukemoid reactions and leukoerythroblastic reaction, among others. In bacterial infections there may be slight deviations to the left (presence of crooks). Erythroblasts can also be seen in some anemias.
References
- Blood and hematopoietic tissue. Available at: sld.cu
- Gomez A, Casas M. 2014. Angel. Clinical interpretation of the laboratory. 8th Edition. Panamerican Medical Publishing House.
- Solari Soto L, Soto Tarazona A, Mendoza Requena D, Llanos Accounts A. Comparison of parasitic densities in thick venous blood drop versus acupressure in the diagnosis of Malaria vivax. Rev Med Hered 2002; 13 (4): 140-143. Available at: scielo.org.
- Terry Leonard Nelson, Mendoza Hernández Carlos. Importance of the study of the peripheral blood smear in the elderly. Medisur 2017; 15 (3): 362-382. Available at: scielo.sld
- Grinspan S. The study of the peripheral blood smear. Continuing medical education. Available at: bvs.hn/RMH



Yet No Comments