
Hematopoiesis phases and functions
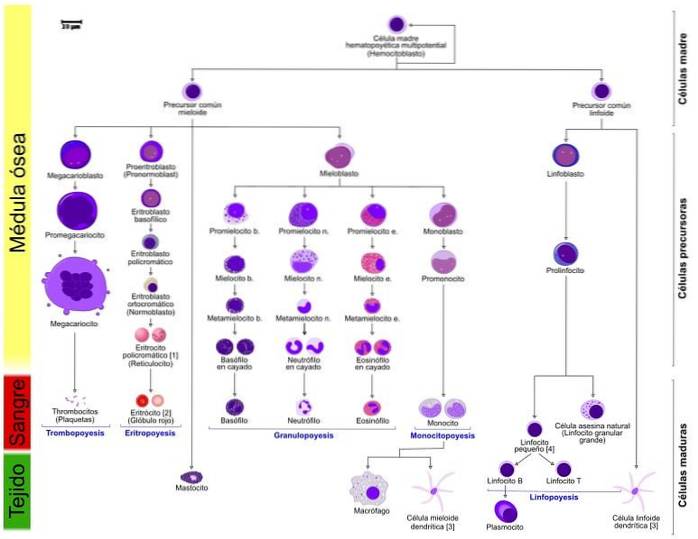
The hematopoiesis is the process of formation and development of blood cells, specifically of the elements that compose it: erythrocytes, leukocytes and platelets.
The area or organ responsible for hematopoiesis varies depending on the stage of development, whether it is embryo, fetus, adult, etc. In general, three phases of the process are identified: mesoblastic, hepatic and medullary, also known as myeloid..
Hematopoiesis begins in the first weeks of the embryo's life, and takes place in the yolk sac. Subsequently, the liver steals the leading role and will be the site of hematopoiesis until the baby is born. During pregnancy, other organs may also be involved in the process, such as the spleen, lymph nodes, and thymus..
At birth, most of the process takes place in the bone marrow. During the first years of life, the "phenomenon of centralization" or Newman's law occurs. This law describes how the hematopoietic marrow is limited to the skeleton and the ends of the long bones..
Article index
- 1 Functions of hematopoiesis
- 2 phases
- 2.1 Mesoblastic phase
- 2.2 Hepatic phase
- 2.3 Secondary organs in the hepatic phase
- 2.4 Medullary phase
- 3 Hematopoietic tissue in the adult
- 3.1 The bone marrow
- 4 Myeloid line of differentiation
- 4.1 Erythropoietic series
- 4.2 Granulomonopoietic series
- 4.3 Megakaryocytic series
- 5 Regulation of hematopoiesis
- 6 References
Functions of hematopoiesis
Blood cells live for a very short time, on average several days or even months. This time is relatively short, so blood cells must be constantly produced..
In a healthy adult, the production can reach about 200,000 million erythrocytes and 70,000 million neutrophils. This massive production takes place (in adults) in the bone marrow and is called hematopoiesis. The term derives from the roots hemat, what does blood mean and poiesis what does training mean.
Lymphocyte precursors also originate in the bone marrow. However, these elements almost immediately leave the area and migrate to the thymus, where they carry out the maturation process - called lymphopoiesis..
Similarly, there are terms to individually describe the formation of blood elements: erythropoiesis for erythrocytes and thrombopoiesis for platelets..
The success of hematopoiesis depends mainly on the availability of essential elements that act as cofactors in indispensable processes, such as the production of proteins and nucleic acids. Among these nutrients we find vitamins B6, B12, folic acid, iron, among others.
Phases
Mesoblastic phase
Historically, the entire process of hematopoiesis was believed to take place in the blood islets of the extra-embryonic mesoderm in the yolk sac.
Today, it is known that only erythroblasts develop in this area, and that hematopoietic stem cells or stem cells arise in a source near the aorta.
In this way, the first evidence of hematopoiesis can be traced to the mesenchyme of the yolk sac and the fixation pedicle..
The stem cells are located in the liver region, approximately at the fifth week of gestation. The process is transitory and ends between the sixth and eighth week of gestation.
Liver phase
From the fourth and fifth weeks of the gestation process, erythoblasts, granulocytes and monocytes begin to appear in the liver tissue of the developing fetus..
The liver is the main organ of hematopoiesis during the life of the fetus, and manages to maintain its activity until the first weeks of the baby's birth..
In the third month of embryo development, the liver peaks in erythropoiesis and granulopoiesis activity. At the end of this brief stage, these primitive cells disappear in their entirety.
In adults, hematopoiesis in the liver may be activated again, and we speak of extramedullary hematopoiesis.
For this phenomenon to occur, the body has to face certain pathologies and adversities, such as congenital hemolytic anemias or myeloproliferative syndromes. In these cases of extreme need, both the liver and the vessel can resume their hematopoietic function.
Secondary organs in the hepatic phase
Subsequently, megakaryocytic development occurs, together with the splenic activity of erythropoiesis, granulopoiesis and lymphopoiesis. Hematopoietic activity is also detected in the lymph nodes and thymus, but to a lesser degree.
A gradual decrease in splenic activity is observed and with this the granulopoiesis ends. In the fetus, the thymus is the first organ that is part of the lymphatic system to develop.
In some species of mammals, the formation of blood cells in the spleen can be demonstrated throughout the life of the individual.
Medullary phase
Around the fifth month of development, the islets located in the mesenchymal cells begin to produce blood cells of all types.
Spinal production begins with ossification and the development of marrow within the bone. The first bone to exhibit spinal hematopoietic activity is the clavicle, followed by the rapid ossification of the rest of the skeletal components..
An increased activity is observed in the bone marrow, generating an extremely hyperplastic red marrow. By the middle of the sixth month the medulla becomes the main site of hematopoiesis.
Hematopoietic tissue in the adult
Bone marrow
In animals, the red bone marrow or hematopoietic bone marrow is responsible for the production of blood elements.
It is located in the flat bones of the skull, sternum and ribs. In longer bones, the red bone marrow is restricted to the extremities.
There is another type of marrow that is not so biologically important, since it does not participate in the production of blood elements, called yellow bone marrow. It is called yellow because of its high fat content.
In cases of need, the yellow bone marrow can transform into red bone marrow and increase the production of blood elements.
Myeloid line of differentiation
It comprises the maturation cell series, where each one ends in the formation of the different cellular components, whether erythrocytes, granulocytes, monocytes and platelets, in their respective series.
Erythropoietic series
This first line leads to the formation of erythrocytes, also known as red blood cells. Several events characterize the process, such as the synthesis of the protein hemoglobin - respiratory pigment in charge of oxygen transport and responsible for the characteristic red color of the blood..
The latter phenomenon depends on erythropoietin, accompanied by increased cellular acidophilicity, loss of the nucleus, and disappearance of organelles and cytoplasmic compartments..
Let us remember that one of the most notable characteristics of erythrocytes is their lack of organelles, including the nucleus. In other words, red blood cells are cellular "bags" with hemoglobin inside..
The differentiation process in the erythropoietic series requires a series of stimulating factors to be carried out.
Granulomonopoietic series
The maturation process of this series leads to the formation of granulocytes, which are divided into neutrophils, eosinophils, basophils, mast cells, and monocytes..
The series is characterized by a common progenitor cell called the granulomonocytic colony-forming unit. This differs into the cell types mentioned above (neutrophilic granulocytes, eosinophils, basophils, mast cells and monocytes).
From the granulomonocytic colony-forming unit are derived the granulocytic colony-forming and monocytic colony-forming units. Neutrophilic granulocytes, eosinophils and basophils are derived from the first..
Megakaryocytic series
The goal of this series is the formation of platelets. Platelets are irregularly shaped cellular elements, lacking a nucleus, that participate in the blood clotting processes.
The number of platelets must be optimal, since any unevenness has negative consequences. A low number of platelets represents high bleeding, while a very high number can lead to thrombotic events, due to the formation of clots that obstruct the vessels..
The first platelet precursor to be recognized is called a megakaryoblast. Then it is called megakaryocyte, of which several forms can be distinguished.
The next stage is the promegakaryocyte, a cell larger than the previous one. It becomes a megakaryocyte, a large cell with multiple sets of chromosomes. Platelets are formed by the fragmentation of this large cell.
The main hormone that regulates thrombopoiesis is thrombopoietin. This is responsible for regulating and stimulating the differentiation of megakaryocytes, and their subsequent fragmentation.
Erythropoietin is also involved in regulation, thanks to its structural similarity to the aforementioned hormone. We also have IL-3, CSF and IL-11.
Regulation of hematopoiesis
Hematopoiesis is a physiological process that is strictly regulated by a series of hormonal mechanisms.
The first of these is the control in the production of a series of cytosines whose task is the stimulation of the marrow. These are generated mainly in stromal cells.
Another mechanism that occurs in parallel to the previous one is the control in the production of cytosines that stimulate the marrow.
The third mechanism is based on the regulation of the expression of the receptors for these cytosines, both in pluripotent cells and in those that are already in the process of maturation..
Finally, there is a control at the level of apoptosis or programmed cell death. This event can be stimulated and eliminate certain cell populations.
References
- Dacie, J. V., & Lewis, S. M. (1975). Practical haematology. Churchill livingstone.
- Junqueira, L. C., Carneiro, J., & Kelley, R. O. (2003). Basic histology: text & atlas. McGraw-Hill.
- Manascero, A. R. (2003). Atlas of cell morphology, alterations and related diseases. EYEBROW.
- Rodak, B. F. (2005). Hematology: Fundamentals and Clinical Applications. Panamerican Medical Ed..
- San Miguel, J. F., & Sánchez-Guijo, F. (Eds.). (2015). Hematology. Basic reasoned manual. Elsevier Spain.
- Vives Corrons, J. L., & Aguilar Bascompte, J. L. (2006). Manual of Laboratory Techniques in Hematology. Masson.
- Welsch, U., & Sobotta, J. (2008). Histology. Panamerican Medical Ed..



Yet No Comments