
Characteristic hematochezia and what to do in its presence

The hematochezia It is the expulsion of red, bright, bright and fresh blood during defecation. This blood can be expelled just before defecation, come out mixed with stool, or come out at any time unrelated to defecation. Hematochezia can be a manifestation of gastrointestinal bleeding.
Digestive bleeds can present in various forms, including hematemesis (which is vomiting blood), melena (which is black sticky, foul-smelling stools), hematochezia (fresh blood coming out of the rectum), and as occult blood in stools (which are traces blood mixed with stool).
Hematochezia is generally due to bleeding lesions located below the angle of Treitz (junction between the duodenum and jejunum) and is defined as lower gastrointestinal bleeding. In 90% of cases it is a manifestation of lesions located in the colon.
However, on some occasions it can be the product of massive hemorrhages in higher areas of the digestive tract, which are accompanied by acceleration of intestinal transit, so that the blood has very little contact with the walls of the tube and appears in the rectum as blood. "Not modified".
In adults, diverticulosis, which is a disease characterized by the presence of sacs or bags called diverticula that appear in the walls of the colon due to a weakening of the wall, is one of the most frequent causes of lower gastrointestinal bleeding and hematochezia..
Other common diseases that cause lower gastrointestinal bleeding and hematochezia include hemorrhoids, anal fistulas, polyps, inflammations of the intestine, tumors, and ischemic colitis. Hematochezia can also occur in pediatric patients, from newborn to school age, for different causes.
Article index
- 1 Characteristics of hematochezia
- 1.1 Signs of a lower gastrointestinal bleeding
- 2 What to do in the presence of hematochezia?
- 2.1 Diagnostic procedures
- 3 References
Characteristics of hematochezia
Hematochezia can present as persistent bleeding, a self-limited episode, or a recurrence (recurrence of a disease). It can be accompanied by significant hemodynamic alterations, but this depends on the volume of bleeding.
It is considered “self-limited” if blood pressure, heart rate, and hemoglobin levels are stable and no further bleeding (hematochezia) occurs within 24 hours of the first episode..
It is considered "relapse" when a bleeding episode recurs in a period no longer than ten to fifteen days after the first bleeding event..
Massive intestinal bleeding can be life-threatening. Mortality in these cases is related to the volume and rate of blood loss, associated with the disease that causes it, the age of the patient and the effectiveness of the treatment.
In elderly patients, many bleeding colon lesions can present as melena and not as hematochezia, since intestinal transit is much slower and the blood remains in contact with the digestive tract for longer..
Signs of a lower gastrointestinal bleeding
One of the signs of a gastrointestinal bleeding is hematochezia or expulsion of fresh blood through the rectum. Hemodynamic changes that can accompany intestinal bleeding indicate significant blood loss.
Losses equivalent to a liter of blood or more in a short time are accompanied by a decrease in cardiac output, blood pressure and tachycardia (increased heart rate). Systolic pressure (peak pressure) drops below 100 mmHg and heart rate increases above 100 beats per minute.
The accumulation of blood in the gastrointestinal tract is irritating and increases peristaltic movements, causing diarrhea. If the bleeding comes from the lower intestinal tract, that is, from the jejunum, ileum, colon or rectum, the diarrhea is frankly bloody.
In these cases, the hemoglobin and hematocrit values initially are not the best indicators of acute gastrointestinal bleeding, since the plasma and cell volume losses are proportional.
As plasma volume is replenished, hemoglobin and hematocrit values will reflect the amount of blood loss..
However, these values can be modified by the exogenous replacement of fluids or blood that are used to maintain tissue hydration and correct hemodynamic failures (cardiac output and arterial pressure)..
What to do in the presence of hematochezia?
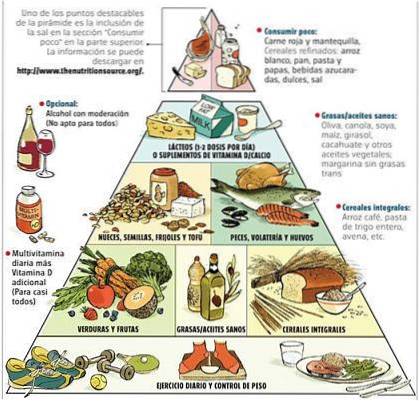
When the presence of blood in the rectum is suspected, first it is necessary to discard some foods or medicines that can stain the stool and simulate glistening blood or melena. Among these we can name beets, liquorice, spinach, blood sausages, medicines such as activated charcoal, iron, some laxatives, rifampicin and food coloring.
Once the previous ones have been discarded, the presence of blood in the rectum must be confirmed, even if it is not very abundant and only the toilet paper wet, the doctor should be consulted.
In the latter case, the inspection of the area and the soft rectal examination procedure that allows detecting fistulas, fissures, veins or indurations, is often enough to make the diagnosis..
When the bleeding has a higher origin, it is necessary to carry out other exploratory tests that will allow a much more precise diagnosis and administer the appropriate treatment..
Diagnostic procedures
Among the most commonly indicated procedures are rectosigmoidoscopy and colonoscopy. They are endoscopic procedures that are used more and more frequently, since they are low-risk procedures and that can be performed on an outpatient basis..
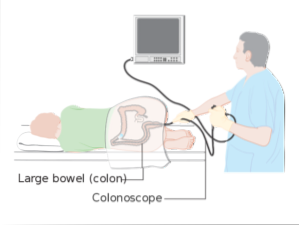
Rectosigmoidoscopy consists of an exam that allows to visualize the mucosa of the lower part of the large intestine, that is, the sigmoid, rectum and anus. A flexible tube equipped with a small camera called a videosigmoidoscope is inserted through the anus, with which, on an external screen, images are transmitted that allow the area to be visualized..
Colonoscopy uses a similar system, but with a tube that is 120-180 cm long. It allows observation of the entire lining of the colon and, if necessary, the lower part of the small intestine. It allows taking biopsies, removing polyps and observing some inflammatory processes, tumors and other diseases of the digestive tract.
Other diagnostic tests are X-rays with contrast, generally barium is used in enemas, which allows visualizing the lower digestive tract. However, colonoscopy is much more versatile and accurate, allowing observation and local treatment if necessary..
References
- Díaz, J. M. P., Pineda, C. L. F., Amaya, R. M., Castañeda, D. O. D., Neira, K. A. C., & Correa, J. G. (2018). Clinical and epidemiological description of patients with ulcerative colitis in a university hospital in Colombia. Medicine, 40(1), 132-133.
- Hauser, S., Longo, D. L., Jameson, J. L., Kasper, D. L., & Loscalzo, J. (Eds.). (2012). Harrison's principles of internal medicine. McGraw-Hill Companies, Incorporated.
- Hung, H. Y., Changchien, C. R., You, J. F., Chen, J. S., Chiang, J. M., Yeh, C. Y.,… & Tasi, W. S. (2006). Massive hematochezia from acute hemorrhagic rectal ulcer in patients with severe comorbid illness: rapid control of bleeding by per anal suturing of bleeder using anoretractor. Diseases of the colon & rectum, 49(2), 238-243.
- Kok, K. Y. Y., Kum, C. K., & Goh, P. M. Y. (1998). Colonoscopic evaluation of severe hematochezia in an Oriental population. Endoscopy, 30(08), 675-680.
- McCance, K. L., & Huether, S. E. (2002). Pathophysiology-Book: The Biologic Basis for Disease in Adults and Children. Elsevier Health Sciences.
- Pincay, C. (2017). Correlation of inflammatory bowel disease with lower digestive bleeding study to be carried out at the University Hospital of Guayaquil, 2014-2016 (Doctoral dissertation, University of Guayaquil. Faculty of Medical Sciences. Medicine career).


Yet No Comments