
Histoplasma capsulatum characteristics, life cycle, pathologies
Histoplasma capsulatum is a fungus considered pathogenic for man and some animals, causing histoplasmosis, a disease capable of producing an intracellular infection of the reticuloendothelial system that can affect almost all tissues or organs of the body.
This infection can be localized benign or systemic fatal. It mainly occurs in its localized form in the lungs, but in some cases it can progress and spread to the lymphatic tissues, spleen, liver, kidneys, central nervous system and skin..
Histoplasmosis is a granulomatous disease that has a wide worldwide distribution, with a high predilection for temperate and tropical zones. Specifically, cases have been reported in America, Africa and Asia, where there are endemic areas. Few cases have been reported in Europe in Italy, Greece, Germany, Belgium, the Netherlands, Denmark and Russia.
However, the highest prevalence is found in mid-North America, along the Mississippi and Ohio Rivers, Missouri, Illinois, Indiana, Kentucky, and Tennessee. At these sites, more than 80% of the population have positive histoplasmin tests, indicating that they have been in contact with the fungus..
Scattered foci are also found in Canada, Mexico, Panama, Guatemala, Honduras, Nicaragua, Colombia, Peru, Bolivia, Brazil, Argentina and Venezuela.
Article index
- 1 Features
- 2 Taxonomy
- 3 Life cycle
- 4 Pathogenesis
- 4.1 Infection in man
- 4.2 Primary acute form
- 4.3 Disseminated form
- 4.4 Chronic cavitary form
- 4.5 Infection in Animals
- 5 Diagnosis
- 5.1 Direct examination
- 5.2 Cultivation
- 5.3 Differential diagnosis
- 5.4 Detection of polysaccharide antigens
- 5.5 Histoplasmin
- 6 Immunity
- 7 Treatment
- 8 References
Characteristics
Histoplasma capsulatum var capsulatum It is a dimorphic fungus, this means that it presents two morphological forms according to the temperature.
In nature (saprophytic life at room temperature) it is found in the form of filaments or hyphae, while in its parasitic life within the body at 37 ° C it occurs in the form of yeast.
The mycelial (filamentous) form of the fungus forms colonies that reproduce by small and large conidia.
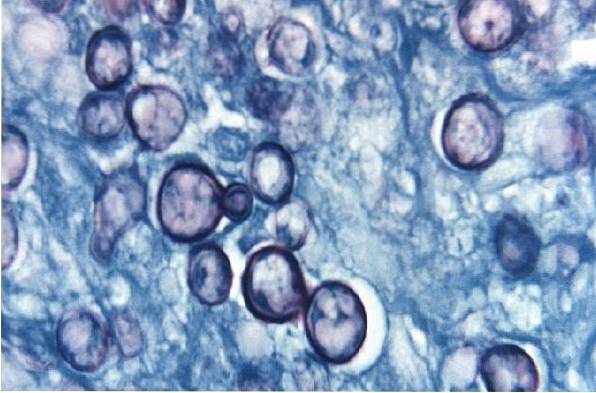
In its yeast form it has a spherical or oval shape and gemstones 2 to 5 µ in diameter. Buds are usually single buds joined by narrow neck.
Yeasts are phagocytosed by alveolar macrophages and within them can travel to all tissues of the reticuloendothelial system.
Within the tissue, the blastoconidia are grouped within the reticuloendothelial cells, since the fungus in its yeast form has an obligate intracellular life, and they are surrounded by a halo similar to a capsule.
Hence, the name of the species is capsulatum, but in itself this name is inadequate, since the fungus as such does not have a capsule.
Taxonomy
Fungi kingdom
Division: Ascomycota
Class: Eurotiomycetes
Order: Onygenales
Family: Ajellomycetaceae
Gender: Histoplasma
Species: capsulatum var capsulatum
Lifecycle
The essential factors that favor the vitality and permanence of the fungus in nature are moderate temperature, relative humidity of 67 to 87% and soils well nourished with organic matter..
The little light in the caves favors the sporulation of the fungus. It is frequently isolated from the ground of poultry pens, such as chicken coops, lofts, as well as the guano of caves or buildings where bats take refuge..
Apparently the droppings of birds or bats contain substances that are nutritious for the fungus, giving a competitive advantage over the rest of the soil microbiota or fauna..
It is believed that the mycophagous mites present in these soils may play a role of dispersal of H. capsulatum, through a pheric mechanism (organism that uses another to transport itself).
These soils, when removed by excavation work, cleaning or by gales that form dust clouds, cause thousands of spores to spread into the air..
This is how humans and animals can inhale the conidia of the fungus, becoming infected. Conidia within the infected individual turn into yeast.
Pathogeny
Infection in man
The disease in humans can be acquired at any age and without distinction of sex, although the disease is more common in men, perhaps because they are more exposed,
Likewise, it does not distinguish between races or ethnicities, while the progressive form of the disease is more frequent in young people..
Laboratory personnel who handle crops or soil to isolate the fungus are permanently exposed to acquiring the infection. Also farmers, builders, archaeologists, guneros, surveyors, miners, cave excavators and speologists.
It is important to note that the disease is not transmitted from one person to another. In man it manifests itself in 3 ways: primary acute form, chronic cavitary form and disseminated form.
Primary acute form
The human inhales the conidia of the fungus, which reach the lungs and after an incubation period of 5 to 18 days a localized lung inflammation occurs when they become yeast.
If the fungus is taken up by dendritic cells, it is destroyed. But if it binds to integrin and fibronectin receptors, and they are taken up by phagocytes, they survive by inhibiting the function of the phagosome-lysosome..
For it, Histoplasma capsulatum fixes iron and calcium to neutralize the acidic pH of the phagolysosome. With continued growth there is lymphatic spread and development of primary lesions.
Later, necrosis occurs, encapsulating or calcifying the lungs. On the other hand, the regional lymph nodes become inflamed, simulating tuberculosis.
Lesions are usually diffuse, discrete, or widely distributed (miliary type) manifested by multiple calcified foci.
In the vast majority of cases, the infection does not progress to the primary stage, leaving only a calcified node as evidence, and the lesions resolve completely..
In other cases, the infection persists and can spread. In this type of infection, the patient may be asymptomatic or may present with certain clinical manifestations such as non-productive cough, dyspnea, chest pain, hemoptysis, and cyanosis..
As in tuberculosis in the lymph nodes, viable cells may remain that can later be reactivated, especially in immunosuppressed.
Disseminated form
A high inhalation load of conidia or repeated exposures is required, the lungs consolidate and the infection progresses hematogenously, producing hepatomegaly and splenomegaly.
The clinical manifestations are fever, digestive disorders, dyspnea, weight loss, anemia, leukopenia, and generalized lymphadenopathy..
Sometimes there are meningitis, endocarditis, intestinal or genital ulcers, and Addison's disease due to involvement of the adrenal glands.
The primary cutaneous presentation causes a painless ulcerated chancre with regional adenopathy; heals on its own in weeks or months.
Polymorphous skin lesions can also be seen: papules; nodules; molluscan, warty, or purpuric lesions; ulcers; abscesses; cellulite, and panniculitis.
Likewise, there may be oral manifestations: painful oropharyngeal ulcers, nodules on the tongue and gums and even the larynx..
Chronic cavitary form
Usually represents a reactivation of a primary lung injury or a form of uninterrupted progression of lung injury.
Here the reticuloendothelial system is involved and the clinical manifestations may be similar to the disseminated form.
Infection in Animals
Various domestic and wild animals can be infected with Histoplasma capsulatum, such as dogs, cats, sheep, geese, rats, mice, mapurites, monkeys, foxes, horses, cattle, among others.
Diagnosis
Depending on the stage of the disease, certain samples may be used for diagnosis such as:
Sputum, gastric lavage, cerebrospinal fluid, citrated blood or bone marrow sample, excision of nodules, urine, liver or spleen puncture.
Direct examination
A direct examination stained with Giensa can be done, when it comes to smears of mucous or skin lesions, smears of lymph node biopsy, smears of blood or bone marrow and puncture of spleen and liver.
On the other hand, Diff-Quick, Pap smear, or Wright stains have been helpful in observing the fungus. In these preparations, the fungus is observed as oval cells of 2 to 4 µ within large mononuclear cells and to a lesser extent within polymorphonuclear cells..
Culture
Histoplasma capsulatum it is developed in enriched media such as blood and chocolate agar or in special medium for fungus such as Sabouraud Agar.
Its growth is slow (10 to 30 days of incubation), between 22 to 25ºC to obtain the form of filamentous fungus. It can be masked by fast growing bacteria or fungi.
The mycelial colony has the appearance of white to tan or brownish gray hair. Delicate, septate hyphae with a diameter of 1 to 2 µm are observed under the microscope and produce microconidia and macroconidia..
Once the colony is mature, the diagnostic form is large, smooth-walled macroconidia at first, then becoming rough and spiny, ranging from 5 to 15 µm in diameter..
This diagnostic form is called tuberculate macroconidia because it has thick-walled, radial finger-like projections..
To demonstrate dimorphism in the laboratory and to pass from the filamentous to the yeast form is a difficult task, but not impossible, successive passages of cultures are needed.
Differential diagnosis
It should be taken into account that in young cultures of samples from skin, the microscopic characteristics of the fungus can be confused with Trichophyton rubrum or Sporothrix schenckii.
This occurs especially if only microconidia are observed, so a differential diagnosis must be made. However, the time and the characteristics of the cultivation clear the doubts.
Detection of polysaccharide antigens
On the other hand, the diagnosis of histoplasmosis can also be made by detecting polysaccharide antigens from H. capsulatum.
This is done using the radioimmunoassay technique in alveolar fluid, urine and blood, useful for both diagnosis and follow-up..
Histoplasmin
It is a delayed hypersensitivity reaction skin test that is only useful in epidemiological studies, as it only tells whether the person has been in contact with the fungus.
Immunity
Neither B lymphocytes nor antibodies confer resistance to reinfection. In this sense, the TH1 lymphocytes are capable of inhibiting intracellular growth and thus controlling the disease..
That is why patients with T lymphocyte deficiency tend to suffer from the disseminated form of the disease. An example is AIDS patients.
On the other hand, of the 5 known serotypes, chemotype II is the most virulent strain, being capable of depressing the production of TNF-α due to the presence of glucans in the cell wall, reducing the host's immune response by blocking a β-glucan receptor known as Dectin-1.
Treatment
Primary disease can resolve without treatment.
In mild disease, itraconazole can be used, and in severe and disseminated form, a cycle of amphotericin B followed by itraconazole is used..
References
- Ryan KJ, Ray C. Sherris. Microbiology Medical, 6th Edition McGraw-Hill, New York, U.S.A; 2010.
- Koneman E, Allen S, Janda W, Schreckenberger P, Winn W. (2004). Microbiological Diagnosis. (5th ed.). Argentina, Editorial Panamericana S.A.
- Forbes B, Sahm D, Weissfeld A. Bailey & Scott Microbiological Diagnosis. 12 ed. Argentina. Editorial Panamericana S.A; 2009.
- Casas-Rincón G. General Mycology. 1994. 2nd Ed. Central University of Venezuela, Library Editions. Venezuela Caracas.
- Arenas R. Illustrated Medical Mycology. 2014. 5th Ed. Mc Graw Hill, 5th Mexico.
- González M, González N. Manual of Medical Microbiology. 2nd edition, Venezuela: Directorate of media and publications of the University of Carabobo; 2011.
- Wikipedia contributors. Histoplasma capsulatum. Wikipedia, The Free Encyclopedia. August 14, 2018, 04:41 UTC. Available at wikipedia.org/
- Histoplasma capsulatum: more widespread than previously thought. Am J Trop Med Hyg. 2014; 90 (6): 982-3.
- Horwath MC, Fecher RA, Deepe GS. Histoplasma capsulatum, lung infection and immunity. Future Microbiol. 2015; 10 (6): 967-75.


Yet No Comments