
Panhypopituitarism causes, symptoms and treatment
The panhypopituitarism It is a condition characterized by the inadequate or absent production of hormones from the anterior pituitary. It can have different manifestations depending on the age at which it appears.
Some of them are short stature, low blood pressure, dizziness, muscle weakness, micropenis, optic atrophy, hypoglycemia, dry skin, fatigue, constipation, etc. However, these symptoms depend on the hormones that are affected and vary if the condition is congenital or acquired..

Panhypopituitarism can have multiple causes. It can appear due to a problem during the embryonic period. Or, due to an injury, inflammation or tumors in older ages.
This disease is chronic and needs permanent treatment to replace the missing hormones. Depending on the deficiency hormones, the indicated treatment will be different. This is based on pharmacological support.
Sometimes the terms hypopituitarism and panhypopituitarism are used interchangeably, although normally the latter concept refers to a total deficiency of certain hormones produced by the anterior lobe of the pituitary gland..
Article index
- 1 Statistics
- 2 Pituitary gland and panhypopituitarism
- 3 Causes
- 3.1 Both hypothalamic and pituitary tumors
- 3.2 Hemochromatosis
- 3.3 Autoimmune diseases
- 3.4 Vascular problems
- 3.5 Empty sella syndrome
- 3.6 Genetic causes
- 3.7 After causes
- 4 Symptoms
- 4.1 Growth hormone deficiency
- 4.2 Gonadotropin hormone deficiency
- 4.3 Thyroid-stimulating hormone deficiency
- 4.4 Adrenocorticotropin or corticotropin deficiency
- 4.5 Prolactin deficiency
- 5 Treatment
- 5.1 Corticosteroids
- 5.2 Testosterone and estrogen
- 5.3 Somatropin
- 5.4 Gonadotropins
- 5.5 Surgery
- 6 Forecast
- 7 References
Statistics
Both hypopituitarism and panhypopituitarism are very rare conditions. There are really few studies examining the prevalence of this condition. Most are focused on hypopituitarism in general.
According to Bajo Arenas (2009), the prevalence of hypopituitarism is 45.5 out of 100,000. There are 4.2 new cases per 100,000 inhabitants..
Pituitary gland and panhypopituitarism
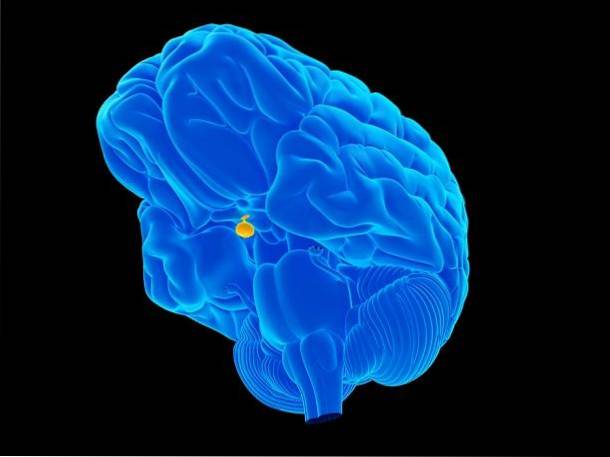
To understand panhypopituitarism, it is important to know the mission of the pituitary gland.
The pituitary gland, also called the pituitary, is the one that is affected in panhypopituitarism. This gland is the "endocrine teacher of the body", since it controls the functions of other endocrine organs..
Thus, it secretes hormones that regulate other important glands, maintaining the homeostasis (balance) of the body. Seeks the proper administration of nutrients and proteins that we get from the diet.
Through hormonal levels, the pituitary gland controls functions such as the growth of the body, hair and nails, body mucous membranes, breast milk, etc..
This gland is located on a bone called the “sella turcica” found in the ephenoid bone of the skull. Thanks to its location, it connects with the hypothalamus more easily, through a structure called the pituitary stalk. The lasts of the hypothalamus control the anterior pituitary.
The pituitary or pituitary is divided into the anterior and posterior lobe. The former produces thyroid stimulating hormone (TSH), corticotropin, luteinizing hormone (LH), follicle stimulating hormone (FSH), growth hormone (GH) and prolactin. While the later secretes vasopressin (antidiuretic hormone) and oxytocin.
In panhypopituitarism, there is an absence of these hormones for various reasons. Therefore, patients who suffer from it may have problems in the functioning of their body.
Causes
Panhypopituitarism can be caused by acquired causes or, less frequently, by genetic causes. When the pituitary gland does not function as it should, but the causes have not yet been identified, it is called "idiopathic panhypopituitarism.".
The most common acquired causes appear to be tumors involving the pituitary gland. The second most common cause is Sheehan syndrome, which occurs in women after childbirth. It is characterized by an infarction in the pituitary gland as a consequence of bleeding during or after childbirth..
The following are most possible causes of panhypopituitarism:
Both hypothalamic and pituitary tumors
In adults, the most common are pituitary adenomas and account for between 10 and 15% of intracranial tumors. They tend to grow slowly and affect women more. However, they do not normally metastasize.
In children, craniopharyngiomas can occur. They are tumors that appear from embryonic remains of Rathke's bag (a structure that during embryonic development gives rise to the pituitary gland). They are manifested by an increase in intracranial pressure, headaches, vomiting, short stature and slow growth.
Hemochromatosis
This is a hereditary disease that affects iron metabolism, producing excessively high levels of iron..
Autoimmune diseases
Autoimmune diseases in which the immune system fails and attacks healthy body tissues. An example is the autoimmune lymphocytic pituitary gland, in which this system destroys the lymphocytes of the pituitary.
Vascular problems
Vascular problems in this gland such as Sheehan's syndrome or internal carotid aneurysm (which supplies the gland).
Empty sella syndrome
Occurs when the pituitary gland shrinks, pressured by an increase in leaked cerebrospinal fluid.
Genetic causes
As genetic mutations in PIT1 or PROP1. A genetic syndrome associated with panhypopituitarism is Kallmann syndrome. It is characterized by the lack of development of sexual characteristics and olfactory alterations.
After causes
- Defects during embryonic development of the cells that make up the anterior pituitary, or hypothalamus.
- Acquired infundibular lesions (at the back of the pituitary gland) after a stroke, for example.
- Metastasis from other tumors, such as breast, prostate, colon, or lung.
- Radiation therapy treatments.
- Granulomatosis (inflammation of blood vessels) involving the area of the pituitary or hypothalamus.
- Infections such as tuberculosis, toxoplasmosis, syphilis, or mycosis.
- Pituitary apoplexy: it is an ischemia or a hemorrhage that affects the pituitary gland. Produces symptoms such as headache, vomiting and visual deficit.
- Sequelae after surgery that affects the pituitary or involved areas.
- Head trauma.
Symptoms
The symptoms of panhypopituitarism vary greatly depending on the causes, age, how quickly it appears, the hormones involved, and the level of severity..
In this way, there may be patients who present with severe hypothyroidism (poor functioning of the thyroid gland), while others only feel general malaise or excessive fatigue..
Obviously, the consequences are worse when panhypopituitarism appears earlier.
Growth hormone deficiency
The absence of hormones produces different symptoms depending on what they are. Thus, a lack of growth hormone (GH) causes short stature in children. While in adults it leads to changes in body shape, glucose and lipid metabolism problems, and general ill feeling.
Gonadotropin hormone deficiency
The deficiency of gonadotropins, on the other hand, would cause a delay in menstruation or lack of it and low libido. In men it produces sexual dysfunction and micropenis (if the problem appears in childhood).
Thyroid-stimulating hormone deficiency
On the other hand, if there is an absence of thyroid stimulating hormones (TSH), hypothyroidism would appear, characterized by weight gain, fatigue, intolerance to cold, muscle aches, constipation, depression, etc..
Adrenocorticotropin or corticotropin deficiency
The lack of adrenocorticotropic hormone or corticotropin (ACTH) has more negative consequences and can endanger the life of the patient. Especially if the deficit occurs abruptly. In this case, it is manifested by low blood pressure, hypoglycemia, nausea, vomiting, extreme fatigue and a low sodium concentration in the blood..
If ACTH levels drop slowly, symptoms are weight loss, weakness, fatigue, and nausea..
Prolactin deficiency
On the other hand, a lack of prolactin is a very telling symptom of panhypopituitarism. It can prevent women from producing milk after pregnancy. It is also a cause of the previously described Sheehan syndrome.
Other general symptoms of panhypopituitarism are hypersensitivity to cold, decreased appetite, anemia, infertility, loss of pubic hair, lack of body hair, facial swelling, inhibited sexual desire, etc..
Excessive thirst and an exaggerated increase in urine secretion, which come from diabetes insipidus, may also appear. The latter condition arises from a deficit of vasopressin, a hormone that is produced in the hypothalamus and stored in the pituitary gland..
Treatment
The main treatment for panhypopituitarism consists of replacing those hormones that are absent or deficient. At the same time that the underlying cause that caused this condition is treated.
The exact doses of hormones will have to be prescribed by an endocrinologist after having carried out the appropriate analyzes. They should be the amounts that the body would naturally manufacture if there were no panhypopituitarism. This hormone replacement can last a lifetime.
Corticosteroids
Corticosteroids such as hydrocortisone or prednisone are often prescribed to replace those hormones that are missing due to corticotropin deficiency (ACTH). They are drugs that are ingested orally two or three times a day.
A drug called levothyroxine is used to replace a deficiency of thyroid stimulating hormone (TSH)..
Testosterone and estrogen
There may be a deficit of sex hormones. To achieve normal levels, men are given testosterone in different ways. For example, through the skin with a patch, with a daily use gel, or by injections.
In women, estrogen and progesterone are added to the body with gels, patches, or pills. Oral contraceptives are the most used in young women, while estradiol valerate is recommended for women close to menopause.
Somatropin
When there is a deficit in growth hormone, it is necessary to inject somatropin under the skin. Those who receive this treatment in adulthood will notice obvious improvements, although they will not increase their height..
Gonadotropins
On the other hand, if there are fertility problems caused by panhypopituitarism, it is possible to inject gonadotropins to stimulate ovulation in women. As well as the generation of sperm in men.
Strict adherence to treatment is important to improve. Like a follow-up over time by an endocrine specialist. This will verify that the treatment is being effective, and that the hormone levels remain within normality..
Surgery
In cases where there are tumors that have produced panhypopituitarism, surgery is necessary to remove them. Whereas, if the pituitary gland is under pressure, a decompression of it can be chosen through transsphenoidal surgery (bypassing the sphenoid bone). This last treatment is the most appropriate to treat pituitary apoplexy.
It has been proven that rapid decompression could partially or completely restore pituitary function. In addition to reducing the need for chronic hormone therapy (Onesti, Wisniewski & Post, 1990).
Forecast
Patients with panhypopituitarism appear to have twice the risk of death. Mainly due to respiratory and cardiovascular affectations. However, if it is detected early and treatment is followed, the patient can lead a normal life.
References
- Bajo Arenas, J.M. (2009). Gynecology Fundamentals. Madrid: Panamerican Medical Ed..
- Chapter 5. 5. Neuroendocrine pathology. Hypopituitarism. (s.f.). Retrieved on January 25, 2017, from Principles of Urgencies, Emergencies and Critical Care: treaty.uninet.edu.
- Contreras-Zúñiga, E., Mosquera-Tapia, X., Domínguez-Villegas, M. C., & Parra-Zúñiga, E. (2009). Sheehan syndrome: description of a clinical case and review of the literature. Colombian Journal of Obstetrics and Gynecology, 60 (4), 377-381.
- Fernández-Rodríguez, E., Bernabeu, I., & Casanueva, F. F. (2012). Hypopituitarism. Panhypopituitarism. Medicine-Accredited Continuing Medical Education Program, 11 (13), 773-781.
- Hoffman, R. (2016, October 18). Panhypopituitarism. Retrieved from Medscape: emedicine.medscape.com.
- Hypopituitarism. (s.f.). Retrieved on January 25, 2017, from Mayoclinic: mayoclinic.org.
- Onesti ST, WisniewskiT, Post KD. Clinical versussubclinical pituitary apoplexy: Presentation, surgical management and outcome in 21 patients. Neurosurgery 1990; 26: 980-986
- Pombo, J. H. (2000). Panhypopituitarism. Medicine-Accredited Continuing Medical Education Program, 8 (16), 855-859.
- Seoane, E. (s.f.). PANHIPOPITUITARISM. Retrieved on January 25, 2017, from the Endrocrinology Chair: catedraendocrinologia.files.wordpress.com.
- Vázquez, M. R., & García-Mayor, R. V. (2002). Epidemiology of hypopituitarism and pituitary tumors. Clinical Medicine, 119 (9), 345-350.



Yet No Comments