
Proerythroblast characteristics, morphology, regulation, staining
The proerythroblast it is the first immature stage of the red cell series identifiable at the bone marrow level. Therefore, it is part of the process called erythropoiesis. The proerythroblast originates from the unipotent cell called the colony-forming unit of the erythroid line (CFU-E).
The proerythroblast is a large cell; its size is 10 times that of the mature erythrocyte. This cell is characterized by presenting a round nucleus, and on some occasions it is possible to observe 2 or more well-defined nucleoli. The cytoplasm has a great affinity for basic dyes and is intensely stained by them..
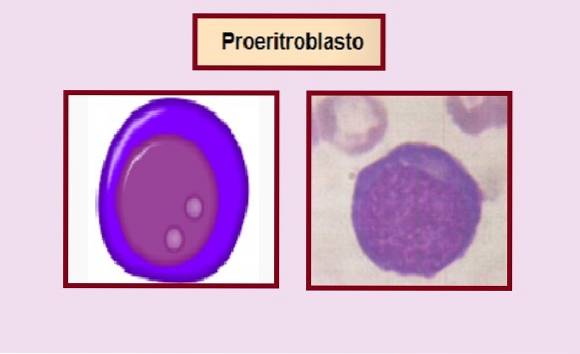
With hematoxylin-eosin staining, the cytoplasm is deep blue. The proerythroblast retains the ability to divide by mitosis that its predecessor possesses and maintains it until the basophilic normoblast stage.
Each proerythroblast during the maturation process is capable of producing a total of 16 to 32 reticulocytes. The proerythroblast maturation process lasts approximately 5 days.
During this period, the cell matures its cytoplasm and its size decreases considerably. During this process, the cell goes through various stages that are: basophilic erythroblast or normoblast, polychromatophilic normoblast and orthochromatic normoblast. Later it expels the nucleus forming the reticulocyte. The maturation process ends when the reticulocyte turns into an erythrocyte.
The whole process occurs within the red bone marrow.
Article index
- 1 Features
- 2 Morphology
- 3 Regulation of proerythroblast proliferation
- 4 Staining
- 5 Pathologies
- 5.1 -Pure aplasia of the red series
- 5.2 -Congenital dyserythropoietic anemias
- 6 References
Characteristics
The proerythroblast is also known by the name of rubriblast or pronormoblast. This cell is an essential precursor in the process of erythropoiesis, known as the process of formation and differentiation of red blood cells or erythrocytes..
Erythropoiesis begins with the differentiation of the committed cell to form cells of the erythroid lineage called BUF-E. This cell differentiates into the colony-forming unit of the erythroid line (CUF-E) and this in turn differentiates into proerythroblast.
The proerythroblast is the penultimate cell in this series with the ability to divide. That is why this cell is a very important precursor in the process of formation and differentiation of erythrocytes or red blood cells..
A total of 16 to 32 mature erythrocytes can originate from each proerythroblast. During the differentiation process, the proerythroblast divides and the cell maturation phase begins. This consists of several recognizable stages: basophilic erythroblast or normoblast, polychromatophilic normoblast, orthochromatic normoblast, reticulocytes, and mature erythrocyte..
Until the orthochromatic normoblast stage, the cell is nucleated, but when the orthochromatic normoblast matures, it expels the nucleus of the cell definitively and becomes an enucleated cell called a reticulocyte, later a mature erythrocyte..
Morphology
The proerythroblast is a large cell, its size is 10 times that of the mature erythrocyte. This cell is characterized by having a round nucleus and it is sometimes possible to observe 2 or more well-defined nucleoli. The cytoplasm has a great affinity for basic dyes and is intensely stained by them..
This cell is often confused with the rest of the blasts present in bone marrow, that is, lymphoblasts, monoblasts, myeloblasts, megakaryoblast.
Regulation of proerythroblast proliferation
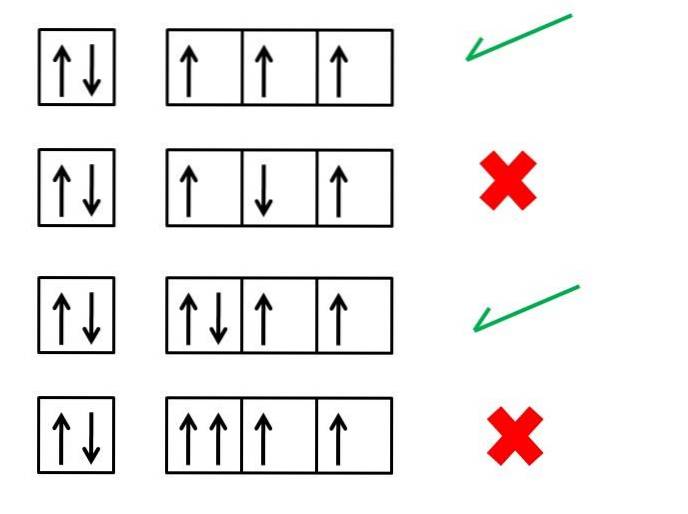
For the process of differentiation and maturation of red blood cells to occur normally, the presence of vitamin B12 and vitamin B9 is necessary. Both are specifically essential for cell division and DNA synthesis..
In this sense, the aforementioned vitamins act directly on the precursors of the erythroid line with division capacity: that is, on BUF-E, CUF-E, proerythroblast and basophilic normoblast..
On the other hand, the proerythroblast has receptors for erythropoietin in its membrane, although in less quantity than its predecessor. Therefore, erythropoietin exerts a regulatory action on erythropoiesis through these cells..
This hormone stimulates the proliferation and differentiation of erythroid precursors (CFU-E and the proerythroblast) in bone marrow, increases the production of hemoglobin and stimulates the release of reticulocytes..
In the specific case of the proerythroblast cell, erythropoietin stimulates mitotic division and transformation to basophilic normoblast. It also induces the accumulation of iron in the cytoplasm, which will serve for the future synthesis of hemoglobin in the later stages..
Likewise, erythropoietin also participates in the regulation of certain genes in these cells. This hormone increases when there is a decrease in oxygen in the tissues.
Staining
Bone marrow and peripheral blood smears are commonly stained with Wright's, Giemsa, or hematoxylin-eosin stains..
The cytoplasm of proerythroblasts is characteristically basophilic. Therefore, with any of these stains the color that it will take will be an intense purplish blue. While the nucleus turns purple.
The intense basophilia helps to differentiate it from the rest of the blasts..
Pathologies
-Pure aplasia of the red series
In pure aplasia of the red series, a selective decrease in the erythroid series is observed, with normal leukocytes and platelets.
This disease can present in an acute or chronic form and the cause can be primary or secondary; primary when it is born and secondary when it is originated as a consequence of another pathology or external factor.
Idiopathic or primary
In the case of primary it is called anemia or Blackfan-Dia-mond syndrome.
In these patients, a hyporegenerative macrocytic anemia is evidenced in peripheral blood. While in bone marrow absence of erythroid precursors is observed.
High school
Sharp
Secondary acute red series pure aplasia can be triggered by viral infections. This is possible only in patients with chronic hemolytic anemia as the underlying disease..
Among the viral infections that can trigger this disease in the mentioned patients are: Parvovirus B19, Hepatitis C virus (HCV), Cytomegalovirus, Epstein-Barr virus, Mumps virus, Measles virus and virus of the human immunodeficiency (HIV).
In the bone marrow of these patients, the typical presence of giant proerythroblasts will be observed..
Another secondary cause may be exposure to environmental toxins or the consumption of certain drugs, such as azathioprine, anti-erythropoietin antibodies, sulfonamides, cotrimoxazole, interferon, among others..
Chronicle
Pure aplasia of the chronic red series is mainly due to the presence of thymomas, autoimmune diseases or lymphoproliferative syndromes, among other causes of neoplastic origin..
It can also be caused by incompatibilities of the ABO system in allogeneic bone marrow transplants..
-Congenital dyserythropoietic anemias
It is a rare disease.
Patients with this disease present a bone marrow with marked hyperplasia in the erythroid series, with asynchrony in the nucleus - cytoplasm maturation process, cloverleaf nuclei, presence of binuclear proerythroblasts, intracytoplasmic inclusions and cells with internuclear bridges..
While in peripheral blood it is characterized by the presence of anisocytosis (especially macrocytosis), poikilocytosis (mainly spherocytes) and hypochromia.
1% erythroblasts and other abnormalities of the erythroid series are also observed, such as: Cabot's ring and basophilic stippling.
References
- Naranjo C. Atlas of Hematology Blood cells. 2nd edition. 2008. Catholic University of Manizales, Mexico. Available at: Users / Team / Downloads / Atlas%.
- "Proerythroblast." Wikipedia, The Free Encyclopedia. 21 Dec 2017, 18:10 UTC. 7 Jul 2019, 23:04 Available at: es.wikipedia.org
- "Erythropoiesis." Wikipedia, The Free Encyclopedia. 29 May 2019, 15:28 UTC. 7 Jul 2019, 23:06 Available at: wikipedia.org/
- Sánchez P, Sánchez A, Moraleda J. (2017). Hematology Undergraduate. 4th Edition. Virgen de la Arrixaca University Clinical Hospital. Murcia. Professor of Medicine. University of Murcia.
- Gutiérrez A, Ramón L, Breña D, Jaime J, Serrano J, Arencibia A, et al. Congenital dyserythropoietic anemia type 1. Presentation of a case. Rev Cubana Hematol Immunol Hemoter 2010; 26 (2): 62-70. Available in: scielo.


Yet No Comments