
Capillary puncture materials, procedure, exams

The capillary puncture it is an alternative way to collect blood samples. There are several anatomical sites where this type of puncture can be performed. These can be on the fingertip, on the heel of the foot, on the forearm, or on the earlobe. The capillary puncture is not the most common way used to draw blood, but it is a good alternative on certain occasions and in particular tests.
The blood obtained from the capillary puncture comes from very small capillary vessels and when trying to stimulate their outflow, it can be accompanied by interstitial and intracellular fluids. Sample collection, to be successful, must be of adequate depth in an area with high blood flow.
Although these techniques are very simple to perform, it is necessary for a professional in the area to take the sample, since if mistakes are made, they can significantly alter the results of some analyzes..
When venous sampling is difficult due to various factors, such as very fine veins, elderly patients, neonates, patients with burned arms, among others, capillary sampling can be a good alternative..
On the other hand, it is an excellent option when the tests to be carried out do not require a large volume of sample (< de 1 ml), por ejemplo: determinación de los niveles de glucosa en sangre y el grupo sanguíneo, entre otros. Así mismo, hay pruebas que solamente pueden realizarse a través de una punción capilar, ejemplo el análisis del tiempo de sangría.
Article index
- 1 Materials for capillary puncture
- 1.1 Materials for sampling
- 1.2 Complete hematology manual
- 1.3 Rapid tests
- 1.4 Blood chemistry or automated hematology
- 2 Procedure
- 2.1 -Capillary sampling on the fingers
- 2.2-Capillary puncture at the heel level
- 2.3 -Puncture in the earlobe
- 2.4 -Puncture in the forearm
- 3 Possible exams
- 3.1 Clotting or bleeding time
- 3.2 Determination of certain analytes
- 4 Precautions
- 5 Recommendations
- 6 References
Materials for capillary puncture
The materials needed to carry out this type of sampling are the following.
Materials for sampling
- Disposable gloves.
- A sterile lancet or an automatic withdrawal or lancing pen.
- Iodized alcohol or povidone-iodine.
- Dry sterile gauze.
The rest of the materials will depend on the analysis to be done.
Complete hematology manual
- Heparinized capillary tubes.
- Hematocrit Sealer.
- Slides.
- Measuring pipettes (for red blood cells, for white blood cells) or automatic pipettes.
Rapid tests
- Test strips.
Blood chemistry or automated hematology
To collect a small volume of blood for other tests, special tubes called “microtainer” are needed..
Process
The collection of blood by capillary puncture is a relatively simple technique. The anatomical sites for sampling are various and are mentioned below.
-Capillary sampling on fingers
Finger selection and puncture site location
Usually the middle or ring finger is chosen. The appropriate area for the puncture is then located (sides of the selected fingertips).
The patient should preferably be seated and the hand should be resting on the armrest of the sampling chair..
To increase blood flow, the patient's fingertip can be gently massaged or the finger can be placed in warm water (no higher than 40 ºC). If the finger is cold or purple (cyanotic), or has signs of inflammation or has a scar, it cannot be used for capillary puncture.

Disinfection of the area
First, the puncture site is disinfected with gauze soaked in iodized alcohol or povidone iodine. Antiseptics should work for at least two minutes.
The puncture should not be performed if the antiseptic has not yet dried, as this will cause interference in the analyzes.
Puncture
- The disposable lancet is uncovered from the opposite end to the tip, in order to prevent it from being contaminated or accidentally punctured.
- The lancet is used very carefully to prick the chosen finger. The movement must be accurate and with a certain impulse to avoid very superficial punctures; but at the same time it should not exceed 2 mm in depth.
It is very important that the lancet is positioned perpendicular to the patient's fingerprints, to avoid wasting blood as it flows through the small grooves of the fingerprints..

Collecting the sample
The blood should flow in the form of a drop, as this will facilitate its collection. If the drops do not flow spontaneously, a slight pressure can be applied to the area, without squeezing or forcing the flow, as this could hemolyze the sample or increase the proportion of interstitial fluids in it..
- The first drop of blood is allowed to lose, because it is contaminated with tissue fluid, and therefore, it must be cleaned with gauze without touching the punctured area.
- The next drops are expected. The objects that can be used to collect the sample can be any of the following:
- Test strip.
- Heparinized capillary tube.
- Slides (for smears).
- Microtainer tubes (small tubes specially designed to collect blood by capillary puncture).
End of sampling
- The puncture site should be pressed with gauze for a few minutes. This can be done by the patient himself if he is an adult or in the case of a child, his representative will do it.
- The lancet must be discarded in a suitable safety container for this purpose and the sample taken to the laboratory.
-Capillary puncture at the heel level
Where it takes place
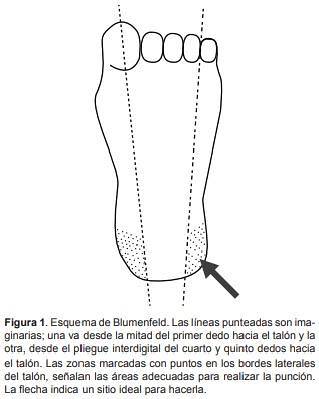
The puncture is made in one of the lateral areas of the heel.
To ensure good blood flow, the area is heated for three to five minutes with a soft towel, moistened with warm water at about 41ºC. The temperature must be controlled so as not to run the risk of burning the patient.
This step is not strictly necessary and can be skipped if there is good irrigation.
Asepsis
The asepsis of the area is carried out preferably using alcohol. The area should be dried using a sterile gauze.
Puncture
The heel is punctured with a disposable lancet, not exceeding 2.4 mm in depth. The first drop will not be collected, therefore, it will be removed with the help of a gauze and then the drops that come later can be collected.
Blood collection
Blood can be collected in special tubes called microtainer or in test strips directly.
In order to increase blood flow, very light pressure may be applied intermittently to the area around the puncture site..
Collect the blood as explained in the capillary sample on the finger.
Last steps
If the blood flow decreases, it should be dried again with gauze and wait for the blood to flow.
Finally, the blood outlet is dried, taking care that the puncture area is not exposed to intense heat, such as by exposure to the sun..
-Puncture in the earlobe
This puncture is done to determine the bleeding time test. To do this, proceed as follows:
Clean and dry the earlobe, without rubbing the edge of the ear. A glass sheet is placed behind the atrial edge, puncturing vertically with the scalpel, or lancet rapidly until the sound of the scalpel is heard against the sheet. Every 30 seconds the blood is collected on the filter paper, without rubbing.
The test will end when the filter paper is not stained with new drops of blood. It is the right time to stop the stopwatch. Then 30 seconds are subtracted from your reading. This is the bleeding time. Normal value: 1 - 3 minutes.

-Puncture in the forearm
This technique is also used to determine the bleeding time. Proceed as follows:
- Put the cuff of a sphygmomanometer around the arm and adjust the pressure to 40 mm of mercury. Wait approximately 1 minute for intracapillary pressure to stabilize.
- With a disposable lancet, make 3 punctures in rapid succession on the front of the forearm, avoiding scars or superficial veins. Start the stopwatch.
- With filter paper, dry gently without rubbing the 3 bleeding points at the same time, every 30 seconds, until they stop bleeding. When they no longer stain the filter paper, the stopwatch stops..
- The bleeding time will be the time marked by the stopwatch minus 30 seconds. Standard value: 2 - 7 minutes
Possible exams
The execution of blood tests is limited with capillary sampling. Among the tests that can be run are the following:
Clotting or bleeding time
This analysis is done through several methods that involve a capillary puncture. Among them are those that can be performed by a puncture in the ear lobe (more used in adults) or in the forearm (Ivy's method, not widely used).
Determination of certain analytes
The analytes that can be measured through test strips or rapid tests are ideal for samples taken by capillary puncture, because they require a very low sample volume. Ex: glycemia, glycosylated hemoglobin (HbA1 C) or cholesterol.
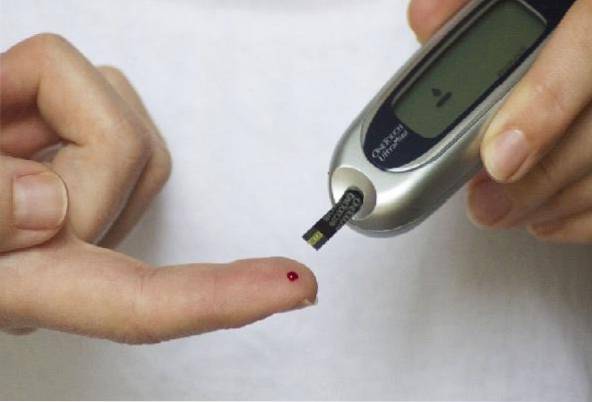
The determination of glycemia by capillary puncture is very frequently used by diabetics to monitor their glucose levels at home. To do this, they use an automatic device called a lancing device..
Complete hematology and platelet count can also be performed.
Precautions
Special care must be taken not to make mistakes in this type of sampling, as it would result in the following:
- Insufficient sample: error in puncture depth and orientation.
- Presence of micro clots in the sample: produced by the delay in the collection, failure in mixing with the anticoagulant, failure in the blood-anticoagulant ratio.
- Dilution of blood with extracellular fluids: by squeezing and forcing the blood flow.
- Serious infections: can occur due to poor asepsis or the use of non-sterile lancets, or repeated punctures in the same site.
- Bone damage - occurs if puncture is too deep or is done in the wrong site.
recommendations
- Fingertip sampling is recommended for patients with difficult veins or burned patients, and for analyzes that do not require large sample volumes. It is not recommended in neonates, as they have very fine and delicate fingers and will not provide the necessary amount of blood..
- Heel puncture is recommended for neonates. However, it is recommended to perform it only when strictly necessary, as it should be considered a painful and uncomfortable method.
Therefore, some laboratories with highly experienced personnel prefer venipuncture, with reduced blood collection, as it is a less painful technique than heel stick..
- Capillary sampling for coagulation tests is not recommended in patients treated with oral anticoagulants, as the INR (International Normalized Ratio) is not standardized for this type of sample collection..
- Always use biosafety measures (gloves, gown, safety glasses), since with this type of tests it is possible that splashes occur.
References
- Vela-Amieva M, Ibarra-González I. Fernández-Lainez C, Belmont-Martínez L. Theoretical-practical foundations for the correct taking of the blood sample from the heel for the neonatal screening. Acta Pediatr Mex 2012; 33 (6): 273-278
- Orellana M, Aramendi M, Martínez P, Sánchez-Calvín M, Galera G., Ribera C. et al. Is it correct to perform the T.A.O. in capillary blood, following the INR criteria in venous blood? Rev Diagn Biol [Internet]. 2002 Dec [cited 2019 May 22]; 51 (4): 131-134. Available at: scielo.org
- Medline Plus. Capillary sample. Available at: medlineplus.gov.
- Sellán M, Díaz M, Vázquez A. Assessment of pain and application of therapeutic nursing interventions in neonatal and pediatric patients, in hospital care contexts. Rev Cubana Enfermer [Internet]. 2012 Jun [cited 2019 May 21]; 28 (2): 144-155. Available at: scielo.org
- Flórez C, Serrano M, Muñoz E, Romero A. Capillary puncture. Manual of general nursing protocols and procedures. 2010. Reina Sofía University Hospital. Available at: juntadeandalucia.es



Yet No Comments