
What is natriuresis?

The natriuresis is the process of increased excretion of the sodium ion (Na+) in the urine through the action of the kidneys. Under normal conditions, the kidney is the main organ that regulates sodium excretion, mainly due to changes in the amount excreted in the urine..
Since the sodium input is not significant in man, the equilibrium must be reached by ensuring that the sodium output equals the sodium input..
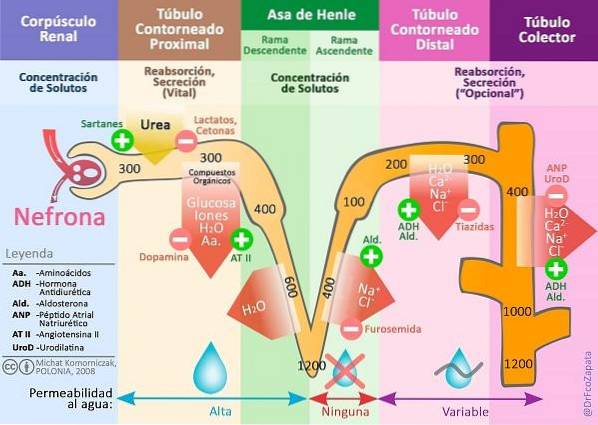
Illustration by: Michał Komorniczak. [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)], from Wikimedia Commons. Translated and modified by the author (@DrFcoZapata)
Article index
- 1 Physiology of water and sodium
- 1.1 -Water
- 1.2 -Sodium
- 1.3 -Regulation
- 2 Altered balance
- 3 Natriuresis and hypertension
- 4 Final considerations
- 5 References
Physiology of water and sodium
Blood volume is the total blood volume of an individual. 55% is the liquid part (plasma) and 45% the solid component (red and white blood cells and platelets). It is regulated by a delicate balance of water and sodium, which in turn regulates blood pressure.
Let's see how this balance occurs.
-Water
On average, 60% of our total body weight is water. The total fluids of our body are distributed in two compartments:
- Intracellular Fluid (ICL). Has 2/3 of the total body water.
- Extracellular Fluid (ECF). It has 1/3 of the total body water and is subdivided into interstitial fluid, plasma and transcellular fluid.
The entry of water into the body is highly variable under normal conditions and must be matched with similar losses to avoid increasing or decreasing the volume of body fluids and therefore blood volume.
90% of the entrance of water to the organism comes given by the ingestion; the other 10% is a product of metabolism.
55% of the water discharge occurs through urine; approximately, another 10% through sweat and feces, and the remaining 35% discharges through what is called "insensitive losses" (of skin and lungs).
-Sodium
Similarly, there must be a balance between sodium intake and output (Na+) in the body. 100% Na+ that enters the body does so through ingested food and liquids.
100% Na+ that discharges does so through urine, since other losses (sweat and feces) can be considered insignificant. Thus, the kidney is the main organ in charge of regulating sodium..
To sustain life, an individual must excrete a long-term amount of Na+ exactly the same as the one you eat.
-Regulation
There is a whole series of regulatory mechanisms that are put in place to keep blood volume (water, sodium and other elements) within its normal limits..
Although they act simultaneously, we will divide them for study purposes into:
Nervous control
Given by the autonomic nervous system, and most of this by the sympathetic nervous system and mediated by norepinephrine, a hormone secreted by the medulla of the adrenal glands.
When there are changes in the intake of fluids and Na+ changes in ECL, blood volume and blood pressure occur simultaneously.
Pressure alterations are the stimulus captured by pressure receptors (baroreceptors) that will produce modifications in the renal excretion of water and Na+ to achieve balance again.
Associated renal and hormonal control
Given by the kidney, adrenals, liver, hypothalamus and pituitary, through a group of hormones: renin-angiotensin-aldosterone system, antidiuretic hormone (ADH or vasopressin), and natriuretic peptides, mainly.
These systems regulate osmolarity (concentration of solutes in the blood). ADH acts at the level of the distal convoluted tubule and collecting tubule (see image above) modifying water permeability and Na transport.+.
Aldosterone, on the other hand, is the main antinatriuretic hormone (which prevents natriuresis). It is secreted when the natraemia (concentration of sodium in the blood) decreases.
It works by causing the reabsorption of Na+ in the final portion of the distal convoluted tubule and collecting tubule, while stimulating the secretion of potassium and protons in the collecting tubule.
Together, angiotensin also regulates renal Na excretion.+ by stimulation of aldosterone production, vasoconstriction, stimulation of ADH secretion and thirst and increased Chlorine and Na reabsorption+ in the proximal convoluted tubule and water in the distal tubule.
Finally, atrial natriuretic peptide (ANP) and a set of similar peptides (brain natriuretic peptide or BNP, type C natriuretic peptide or CNP, type D natriuretic peptide or DNP and urodilatin) increase natriuresis, diuresis and glomerular filtration, while inhibiting renin and aldosterone secretion, and antagonizing the effects of angiotensin and ADH.
Balance disturbance
The mechanisms mentioned very superficially in the previous point will regulate both the excretion of sodium chloride and water and thus maintain blood volume and blood pressure within normal values..
The alteration of all this delicate balance will lead to natriuresis, decreased blood volume (hypovolemia) and arterial hypotension. We are going to observe this alteration in some diseases and syndromes:
- Syndrome of inappropriate antidiuretic hormone secretion
- Salt-wasting syndrome of brain origin
- Diabetes insipidus (nephrogenic or neurogenic)
- Primary or secondary hyperaldosteronism
- Hypovolemic shock.
On the other hand, there are some conditions in which natriuresis is decreased, with the consequent increase in blood volume and resulting hypertension.
This is the case of patients with Nephrotic Syndrome, who deserve the administration of medications such as angiotensin converting enzyme (ACE) inhibitors to increase the excretion of sodium and water, reduce blood volume and thus reduce blood pressure. arterial.

Photo by hywards. Posted on freedigitalphotos.net
Natriuresis and hypertension
There is a concept that has been called "salt-sensitivity" (or sensitivity to salt).
It is of clinical and epidemiological importance as it has been shown to be a cardiovascular risk and mortality factor independent of age and blood pressure levels..
When it is present, there is a genetic alteration at the molecular or acquired level of the renal mechanisms that alter the normal physiology of the regulation of the balance of water and sodium.
It is seen more frequently in elderly people, blacks, diabetics, obese and with kidney dysfunction.
The final consequence is natriuresis with arterial hypertension that is difficult to manage (instead of hypotension), since the physiological (normal) mechanisms that we have already explained are completely counteracted.
Final thoughts
Reducing salt in the diet of salt-sensitive hypertensive patients can allow better control of blood pressure, while reducing the requirement for antihypertensive medications, especially if it is replaced by potassium salts..
It has been suggested that the wide range of effects of natriuretic peptides may be the basis for the development of new therapeutic strategies of great benefit in patients with cardiovascular problems, including coronary artery disease, heart failure and arterial hypertension..
The intrarenal renin angiotensin system is involved in the adjustment of natriuresis and in the hemodynamic effects on glomerular filtration.
In high blood pressure, the consumption of salt (sodium chloride) reduces the activity of the renin angiotensin system; However, in the pathophysiology of salt sensitive hypertension, the determining role of the kidney in the retention of salt at the tubular level is recognized, which conditions the increase in blood pressure.
References
-
- Costa MA, Caniffi C, Arranz CT. Natriuretic peptides. Digital book of the Argentine Society of Arterial Hypertension, Chapter 30. Taken from saha.org.ar
- Raffaelle P. Pathophysiology of hypertension and salt sensitivity. Digital book of the Argentine Society of Arterial Hypertension, Chapter 47. Taken from saha.org.ar
- García GA, Martin D. Physiopathology of hypertension secondary to obesity. Arch Cardiol Mex 2017; 87 (4): 336-344.
- Sánchez R, Ramírez A. Hypertension and sensitivity to salt. Conference at the 7th International Congress of Cardiology of the Argentine Federation of Cardiology. 2017. Taken from: fac.org.ar
- Ardiles L, Mezzano S. Role of the kidney in salt-sensitive hypertension. Rev Med Chile 2010; 138: 862-867.
- Ortega MM. Value of daily natriuresis and its fractionation as a marker of organic damage and in the control of the hypertensive population in primary care.
- Castle ER. Natriuresis and glomerular hemodynamics in a misunderstood renin angiotensin aldosterone system. Rev Med Hered. 2014; 25: 162-167.
- Maicas C, Fernández E et al. Etiology and pathophysiology of essential arterial hypertension. Monocardium 2003; 5 (3): 141-160.
- Herrera J. Salt-dependent hypertension. Arch Cardiol Méx 2001; 71 (Suppl): S76-S80.
- Carbajal-Rodríguez L, Reynes-Manzur JN. Salt-wasting brain syndrome as a differential diagnosis of syndrome of inappropriate antidiuretic hormone secretion. Rev Mex Ped 2000; 67 (3): 128-132.


Yet No Comments