
Arachnoid cyst symptoms, causes and treatment
The arachnoid cyst It consists of a normally benign cavity of cerebrospinal fluid that arises from the arachnoid membrane. It is a rare condition and is usually asymptomatic.
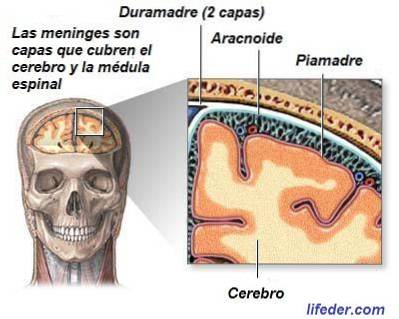
The arachnoid is one of the layers of the meninges, membranes that cover our nervous system to protect and nourish it. Just below it is the subarachnoid space, through which the cerebrospinal fluid circulates. These cysts usually communicate with this space. In addition, they are surrounded by an arachnoid membrane that is indistinguishable from healthy arachnoid..
Arachnoid cysts can appear in both the brain and spinal cord, and contain a clear, colorless fluid that appears to be cerebrospinal fluid, although at other times, it is similar to this.
In some rarer cases it can store xanthochromic fluid. Refers to yellowish cerebrospinal fluid due to the presence of blood that comes from the subarachnoid space.
Article index
- 1 Features
- 2 Discovery of arachnoid cyst
- 3 How to distinguish an arachnoid cyst from other pathologies?
- 4 Causes
- 4.1 Genetics
- 4.2 Cyst growth
- 5 Complications
- 6 Types of arachnoid cysts
- 7 Symptoms
- 7.1 In children
- 7.2 Older children
- 7.3 Chinese doll
- 8 Treatment
- 8.1 Bypassing the liquid
- 8.2 Endoscopic fenestration
- 8.3 Complications in surgeries
- 9 Prevalence
- 10 References
Characteristics
This type of cysts accounts for 1% of space-occupying intracranial lesions in childhood (since they leave the brain without space, pressing it).
They appear mainly in childhood, being very common that it is not diagnosed until adulthood. Many times it is detected in a brain scan incidentally, when the patient was going to have the test for other reasons.
There are two groups of arachnoid cysts according to their nature. Some are primary or congenital, appear due to developmental abnormalities and / or genetic influences.
The others are secondary or acquired, which arise after a complication or are the consequence of another condition. They are less common than the former. For example: head injuries, neoplasms, hemorrhages, infections, surgeries ... the latter are also called leptomeningeal cysts.
An arachnoid cyst usually does not cause symptoms, even if it is large. In the case in which it produces symptoms, these consist mainly of headache, bulging skull (in children), and seizures.
There is a great debate among experts about the treatment of these cysts. Some argue that only patients with symptoms should be treated, while others believe that it is appropriate to intervene in asymptomatic patients to prevent complications.
The most common treatment is based on surgical techniques. Among them, the most used are cystoperitoneal bypass and cyst fenestration. They can be performed by craniotomy or by endoscopic techniques.
Arachnoid cyst discovery
The first author to describe cerebral arachnoid cysts was Richard Bright in 1831. Specifically, he added it in the second volume of his "Reports of Medical Cases." He spoke of them as serous cysts linked to the arachnoid layer.
Later arachnoid cysts were also called "serous meningitis", "brain pseudotumors" or "chronic arachnoiditis".
Later, in 1923, Demel made a review of arachnoid cysts in the literature. He found that the best treatment was trepanation with drainage or removal of the cyst (Vega-Sosa, Obieta-Cruz and Hernández Rojas, 2010).
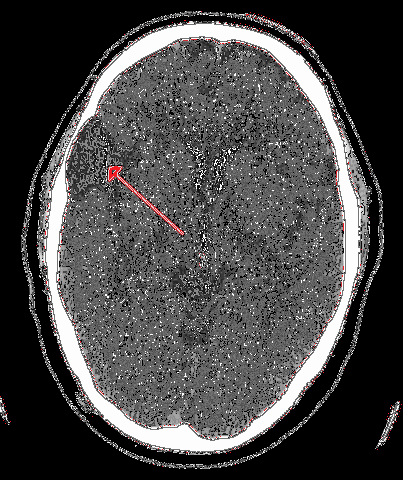
Before the 1970s, arachnoid cysts were only diagnosed when they produced symptoms in the patient. The diagnosis was carried out through cerebral angiography or by a pneumoencephalogram.
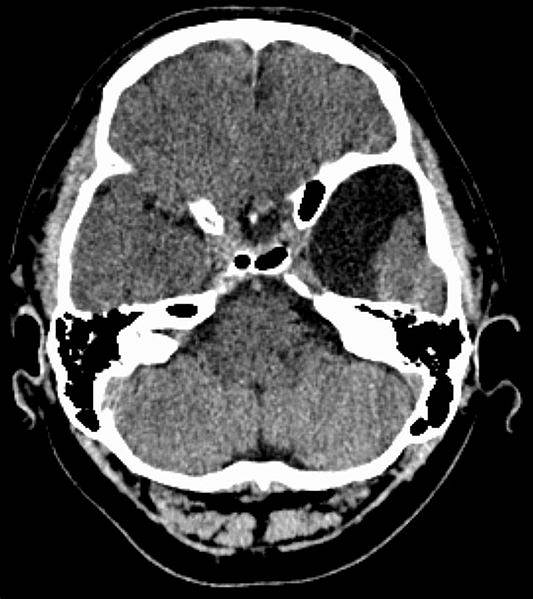
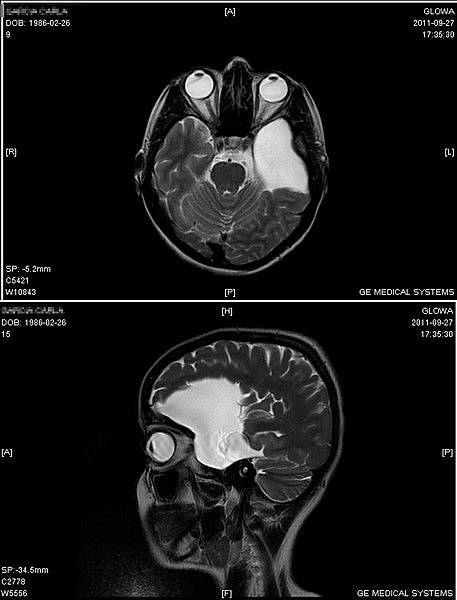
However, after the introduction of neuroimaging techniques such as Computerized Axial Tomography (CT), Magnetic Resonance (MRI) and Ultrasonography (US), the number of cases diagnosed with arachnoid cysts increased.
Thus it was discovered that there are a large number of cases in which cysts are present, but do not cause symptoms. This produced an increase in interest in the study of this condition, mainly its causes and its treatment..
How to distinguish an arachnoid cyst from other pathologies?
Sometimes the arachnoid cyst can be easily confused with atrophied parts of brain tissue, alterations in cisternae of the base, or larger subarachnoid spaces than necessary..
According to Miyahima et al. (2000) the characteristics of an arachnoid cyst are:
- It is located within the arachnoid.
- It is lined by membranes made up of arachnoid cells and collagen.
- They have inside a liquid similar to cerebrospinal fluid.
- The cyst is surrounded by normal arachnoid tissue and.
- It has an external and an internal wall.
Causes
If the arachnoid cyst is primary (that is, it is not a consequence of other damage or complication), its exact cause is not completely known. Apparently, during the development of the fetus in the womb, the arachnoid cyst can develop due to some anomaly in the process.
On the 35th day of gestation, the different layers that cover the brain begin to form: pia mater, arachnoid mater, and dura mater. While, around the fourth month, the subarachnoid space is formed.
At that point, part of the fourth ventricle, a cavity that encloses cerebrospinal fluid, is perforated so that it reaches the subarachnoid space. But, since the arachnoid is not completely differentiated at this stage, a false pathway can be created that fills with fluid. This would form a kind of bag that, if enlarged, will be identified as an arachnoid cyst.
Genetics
On the other hand, there are authors who have found a relationship between arachnoid cyst and genetic predisposition, since they have observed that there are families in which this condition is repeated among its members..
In some cases, an association has been found between the appearance of arachnoid cysts and other systemic malformations such as chromosome 12 trisomy, polycystic kidney, neurofibromatosis or glutaric aciduria type I.
Arachnoid cysts also commonly occur in Chudley-McCullough syndrome, an inherited autosomal recessive disorder. It is characterized by hearing loss, alterations in the corpus callosum, polymicrogyria (many folds on the brain surface, but shallow); cerebellar dysplasia, and enlarged ventricles.
Cyst growth
As for the growth of the cyst, the most accepted theory that explains it is the entry without exit of the liquid. That is, valve mechanisms are formed that cause the fluid from the subarachnoid space to enter the cyst, but not exit.
On the other hand, the arachnoid cyst can be secondary. That is, it arises from trauma (fall, blow or injury), diseases such as inflammations or tumors, or complications after brain surgeries. They can also appear as a consequence of Marfan syndrome, absence (agenesis) of the corpus callosum or arachnoiditis.
Complications
There are complications associated with arachnoid cysts. Trauma can cause fluid within a cyst to leak into other parts of the brain..
The blood vessels on the surface of the cyst could also rupture, causing intracystic hemorrhage, increasing its size. In this case, the patient may suffer symptoms of increased intracranial pressure.
Types of arachnoid cysts
Arachnoid cysts can be classified according to their size or location.
Galassi et al. (1980) differentiated arachnoid cysts of the middle cranial fossa (the part that covers the temporal lobes of the brain) into 3 different types:
- Type 1: are located in the anterior part of the temporal lobe.
- Type 2: They are medium in size, and are found in the anterior and middle part of the fossa. They tend to compress the temporal lobe.
- Type 3: are large cysts of round or oval shape, and cover the entire temporal fossa.
Symptoms
Most arachnoid cysts do not cause symptoms. However, when they form masses that occupy space, produce compression in brain tissue or impede adequate circulation of cerebrospinal fluid, they begin to produce symptoms..
Symptoms depend on age, and the size and location of the arachnoid cyst. The most common are headaches, seizures, and other typical symptoms of hydrocephalus (accumulation of fluid in the brain). For example, drowsiness, blurred vision, nausea, coordination problems, etc..
In children
When children are young, the bones of the skull are still flexible and have not fully closed. This allows their brain to continue to grow without being encased by the skull..
At this stage, an arachnoid cyst would cause an abnormal bulge or enlargement of the head. In addition, in these there is a delay in psychomotor development, visual atrophy and endocrine problems that affect growth..
If the cysts are in the posterior fossa, symptoms tend to appear during infancy and childhood. They normally produce hydrocephalus due to interruption of the circulation of cerebrospinal fluid and symptoms associated with compression of the cerebellum.
Older children
In more advanced stages of development, once the skull is formed, the arachnoid cyst compresses or irritates the brain tissues. Hydrocephalus may appear.
In older children, the main symptom is headache, which occurs in 50% of cases. Seizures appear in 25%. When the arachnoid cyst reaches a large size, it can increase intracranial pressure and cause certain motor disturbances.
Chinese doll
A rare but very typical symptom of an arachnoid cyst is the "Chinese wrist sign", where the patient presents irregular and uncontrolled movements of the head up and down. They arise when sitting and stop when sleeping.
Treatment
Currently there are various positions on the treatment of arachnoid cyst. Many professionals argue that if the cysts are small or do not produce symptoms, surgical interventions should not be performed. Rather, check-ups would be carried out to verify that the cyst is not causing complications..
Instead, when they produce symptoms, have reached a large size or could lead to other problems, a surgical treatment is chosen. The goal of this treatment is to decompress the cyst.
These interventions are about the puncture and aspiration of the cyst, the fenestration (making an incision) in the cyst, and the communication of this with the subarachnoid space, where the cerebrospinal fluid is.
This can be done by craniotomy (removing a small part of the skull) or by endoscopy (inserting an endoscope into the cyst area through a small hole in the skull)..
Bypass of the liquid
Surgeons may also choose to divert the fluid from the cyst to other cavities where it can be reabsorbed..
For example, it may be effective to place a cystoperitoneal shunt so that fluid gradually empties into the peritoneum, avoiding sudden decompression of the brain that could lead to complications..
Endoscopic fenestration
Endoscopic fenestration is the best therapeutic option that exists today, since it is minimally invasive, does not require the implantation of foreign materials and has a relatively low rate of complications, especially when the fluid is diverted to the ventricles and cerebral cisterns.
Complications in surgeries
On the other hand, it is necessary to highlight that the complications of the surgical treatment of the arachnoid cyst are related to its location and size, rather than to the method used..
Some of the complications that Padrilla and Jallo (2007) found in their patients after surgery were spasticity (very tense muscles), hemiparesis (paralysis or weakness on one side of the body), loss of cerebrospinal fluid, hydrocephalus or subdural hygroma.
There were no deaths in these cases, as in several other studies that performed similar interventions.
Prevalence
Arachnoid cysts appear to account for approximately 1% of all intracranial space-occupying lesions. While, in 0.5% of autopsies they have been discovered incidentally.
Most are detected in the first 20 years of life, since they tend to have a congenital origin. In fact, between 60 and 90% of patients are under 16 years of age. In older adults and the elderly it is much less common. Around 10% of these patients may have more than one lesion associated with the cyst.
Regarding the location, between 50 and 60% of arachnoid cysts appear in a region called the middle cranial fossa. These are more common in men than in women, and are usually on the left side. They are usually due to alterations in development.
However, these cysts can proliferate in any area of the nervous system where the arachnoid layer is. Therefore, it is also common for them to arise below the ventricular system, near the aqueduct of Silvio. Other sites consist of the suprasellar region (10%), the convexity (5%), the interhemisphere (5%), and the intraventricular space (2%)..
Others can be located in the posterior fossa, highlighting those associated with the vermis and the cisterna magna (12%). They have also been found in the cerebellopontine angle (8%), the quadrigeminal lamina (5%) and the prepontine space (1%) (Vega-Sosa, Obieta-Cruz and Hernández Rojas, 2010).
On the other hand, arachnoid cysts can manifest within the spinal canal, surrounding the spinal cord. They can be found in the extradural or intradural space (epidural space).
Spinal arachnoid cysts tend to be misdiagnosed as symptoms are often ambiguous. If they produce symptoms of spinal compression, it is important to do an MRI and remove the cysts surgically.
References
- Arachnoid Cyst Imaging. (January 5, 2016). Obtained from MedScape: emedicine.medscape.com.
- Arachnoid Cysts. (s.f.). Retrieved on January 14, 2017, from NORD: rarediseases.org.
- Arachnoid Cysts / Intracranial Cysts. (June 2015). Retrieved from Weill Corner Brain and Spine Center: weillcornellbrainandspine.org.
- Cabrera, C. F. (2003). Cerebrospinal fluid and lumbar puncture in the 21st century. Rev Postgrad VI a Cátedra Med, 128, 11-18.
- Gaillard, F. (s.f.). Simple intraventricular cysts. Retrieved on January 14, 2017, from Radiopaedia: radiopaedia.org.
- Goyenechea Gutiérrez, F. (s.f.). Arachnoid cysts. Retrieved on January 14, 2017, from Red de Salud de Cuba: sld.cu.
- Pradilla, G., & Jallo, G. (2007). Arachnoid cysts: case series and review of the literature. Neurosurgical focus, 22 (2), 1-4.
- Vega-Sosa, A., de Obieta-Cruz, E., & Hernández-Rojas, M. A. (2010). Intracranial arachnoid cysts. Cir Cir, 78 (6), 556-562.


Yet No Comments