
Myotatic reflex elements, physiology and functions

The myotatic reflex, Also known as “stretch reflex” or “osteotendinous reflex”, it is a neurological phenomenon during which a muscle or group of muscles contracts in response to the sudden and abrupt stretching of its insertion tendon in the bone.
It is an automatic and involuntary response integrated at the level of the spinal cord, that is, the individual has no control over the response, which will appear whenever the corresponding stimulus is present (unless there is a lesion that compromises the reflex ).
The myotatic reflex is of clinical utility since it allows evaluating not only the indemnity of the reflex arc itself, but also the integrity of the superior medullary segments.
Outside of clinical practice, in the context of everyday life, the myotatic reflex secretly protects the muscles of the extremities without the people noticing, avoiding the excessive stretching of the muscle fibers under loads, the latter being key also for basal muscle tone and balance.
Article index
- 1 Reflex arc (elements)
- 1.1 Receiver
- 1.2 Afferent (sensory) pathway
- 1.3 Integration
- 1.4 Efferent (motor) pathway
- 1.5 Effector
- 2 Physiology of the myotatic reflex
- 3 Muscles with myotatic reflex
- 4 Examination of the myotatic reflex
- 5 Function of the myotatic reflex
- 6 References
Reflex arc (elements)

Like any other reflex, the myotatic reflex is an "arch" made up of five key elements:
- Receiver
- Afferent pathway (Sensitive)
- Integration core
- Efferent (motor) pathway
- Effector
Each of these elements has a fundamental role in the integration of the reflection and the damage to any of them leads to its abolition..
Detailed knowledge of each of the elements that make up the tendon reflex is crucial, not only to understand it but also to be able to explore it..
Receiver
The receptor and initiator of the myotatic reflex is a complex of sensory fibers located inside the muscles known as the "neuromuscular spindle".
This group of nerve fibers are able to detect changes in the level of stretching of the muscle, as well as the speed of stretching; in fact, in the neuromuscular spindle there are two types of sensory fibers.
Type I afferent neurons respond to small, rapid changes in muscle length, whereas type II neurons respond to larger length changes over a longer period of time..
Afferent (sensory) pathway
The axons of the neurons located in the neuromuscular spindle join the sensory (afferent) portion of the sensory nerve corresponding to that given muscle, and reach the posterior horn of the spinal cord where they synapse with the interneuron (intermediate neuron)..
Integration
The reflex is integrated into the spinal cord, where the afferent pathway synapses with the interneuron, which in turn connects with the lower motor neuron (a motor neuron located in the spinal cord)..
However, before synapsing with the lower motor neuron, the interneuron also connects with fibers from the lower and upper spinal segments, creating a “chain” of connections between the different spinal levels..
Efferent (motor) pathway
The efferent pathway is made up of the axons of the lower motor neuron, which emerge from the anterior horn of the spinal cord, forming the motor portion of the nerve fillets responsible for the innervation of the muscle..
These axons travel through the thickness of the motor nerve to synapse with the effector located in the muscle where the afferent sensory fibers originated..
Effector
The effector of the myotatic reflex is composed of the gamma motor fibers that are part of the neuromuscular spindle, as well as nerve fillets that go directly to the extrafusal fibers.
The reflex pathway ends at the neuromuscular plate where the motor nerve connects to the muscle..
Physiology of the myotatic reflex
The physiology of the myotatic reflex is relatively simple. First, the stretching of the fibers of the neuromuscular spindle must be given by an external or internal stimulus..
As the neuromuscular spindle stretches, it releases a nerve impulse that travels through the afferent pathway to the posterior horn of the spinal cord, where the impulse is transmitted to the interneuron..
The interneuron is modulated by higher medullary centers and synapses with the lower motor neuron (sometimes more than one), amplifying the signal, which is transmitted through the motor nerve to the effector..
Once back in the muscle, the contraction is triggered by the stimulus generated by the gamma fibers at the level of the neuromuscular spindle, which is capable of “recruiting” more motor units, amplifying the contraction of more myofibrils..
Likewise, and in parallel, the direct contraction of the extrafusal fibers (beta fibers) is stimulated, also in this case the phenomenon of "recruitment", that is, each muscle fiber that contracts stimulates the adjacent fiber, thus amplifying the effect..
Muscles with myotatic reflex
Although the myotatic reflex can be seen in virtually any skeletal muscle, it is much more evident in the long muscles of the upper and lower extremities; thus, in the clinical examination, the reflexes of the following muscles are of interest:
Superior member
- Bicipital reflex (biceps brachii tendon)
- Triceps reflex (triceps tendon)
- Radial reflex (long supinator tendon)
- Ulnar reflex (tendon of the ulnar muscles)
Lower member
- Achilles reflex (Achilles tendon)
- Patellar reflex (joint patellar tendon of the quadriceps femoris muscle)
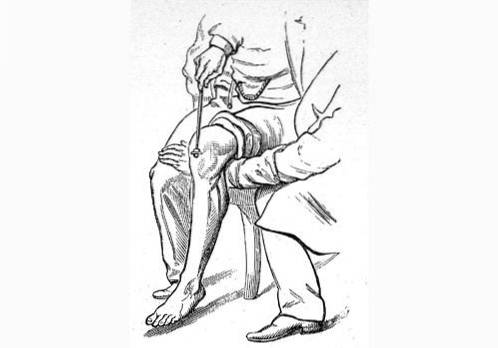
Examination of the myotatic reflex
The exploration of the myotatic reflex is very simple. The patient should be placed in a comfortable position, where the limb is in semi-flexion, without voluntary contraction of the muscle groups.
Once this is done, the tendon to be explored is struck with a rubber reflex hammer. The percussion should be strong enough to stretch the tendon but without causing pain..
The response to the stimulus must be the contraction of the muscle group studied.
According to the clinical finding, the myotatic reflex or tendon reflex (ROT) is reported in the history as follows:
- Areflexia (no response)
- ROT I / IV (grade I over IV osteotendinous reflex) or hyporeflexia (there is response but very weak)
- ROT II / IV (this is the normal response, there should be a perceptible contraction but without generating significant movement of the limb)
- ROT III / IV, also known as hyperreflexia (in response to the stimulus there is a vigorous contraction of the muscle groups involved, with significant movement of the limb)
- ROT IV / IV, also known as clonus (after stimulating the tendon there are repetitive and sustained contractions of the involved muscle group, that is, the stimulus-contraction pattern is lost and the stimulus-contraction-contraction-contraction pattern is exhausts the reflex)
Function of the myotatic reflex
The muscle reflex is extremely important for maintaining muscle tone, regulating balance, and preventing injury..
In the first instance, the degree of elongation of the muscle fibers allows, through the myotatic reflex, that there is an adequate and balanced muscle tone between agonist and antagonist muscles, thus maintaining an adequate posture..
On the other hand, when an individual is incorporated the natural rocking of the body causes the muscle fibers of the muscle group that is on the opposite side of the rocking to elongate. For example:
If a person leans forward, the fibers of the muscles in the posterior region of the leg will elongate. This causes the muscles to contract just enough to correct the sway and thus help maintain balance..
Finally, when a neuromuscular spindle is elongated too much or too fast in response to an effort, what is known as the “reverse myotatic reflex” occurs, which is intended to prevent the rupture of muscle fibers and tendons..
In these cases, the elongation, instead of inducing a muscle contraction, does the opposite, that is, it induces relaxation in order to avoid overloading the muscles beyond their resistance limit..
References
- Schlosberg, H. (1928). A study of the conditioned patellar reflex. Journal of Experimental Psychology, eleven(6), 468.
- Litvan, I., Mangone, C. A., Werden, W., Bueri, J. A., Estol, C. J., Garcea, D. O., ... & Bartko, J. J. (1996). Reliability of the NINDS myotatic reflex scale. Neurology, 47(4), 969-972.
- Golla, F. L., & Antonovitch, S. (1929). The relation of muscular tonus and the patellar reflex to mental work. Journal of Mental Science, 75(309), 234-241.
- Allen, M. C., & Capute, A. J. (1990). Tone and reflex development before term. Pediatrics, 85(3), 393-399.
- Cohen, L. A. (1953). Localization of stretch reflex. Journal of Neurophysiology, 16(3), 272-285.
- Shull, B. L., Hurt, G., Laycock, J., Palmtag, H., Yong, Y., & Zubieta, R. (2002). Physical examination. Incontinence. Plymouth, United Kingdom: Plymbridge Distributors Ltd, 373-388.
- Cohen, L. A. (1954). Organization of stretch reflex into two types of direct spinal arcs. journal of Neurophysiology, 17(5), 443-453.



Yet No Comments