
Serratia marcescens characteristics, pathology and symptoms
Serratia marcescens It is a Gram negative rod, an opportunistic pathogen belonging to the Enterobacteriaceae family. This bacterium was formerly known by the name of Bacillus prodigiosus, but later it was renamed as Serratia marcescens.
The marcescens species is the most important of the Serratia genus, because it has been associated with a wide variety of opportunistic infections in humans. At one time this microorganism was used as a harmless marker of environmental contamination, but today it is considered an invasive microorganism.
It is known that in recent decades it has been wreaking havoc on the hospital environment, especially in intensive care rooms and checkpoints. It has been isolated from sputum samples and blood cultures in patients receiving chemotherapy. Also in urine and CSF samples.
Therefore, it has been the causative agent of pneumonia, septicemia, urinary tract infections, infantile meningitis, among others. Some outbreaks have been caused by the contamination of solutions, objects and instruments for hospital use.
However, outside the nosocomial environment it can also cause infection. It has been seen that 8% of cases of ulcerative keratitis are caused by Serratia marcescens. In addition, it has been associated with the deterioration of some foods rich in starch.
Article index
- 1 Features
- 1.1 General characteristics and growing conditions
- 1.2 Biochemical characteristics
- 1.3 Virulence factors
- 1.4 Antimicrobial resistance
- 2 Taxonomy
- 3 Morphology
- 4 Pathologies and symptoms
- 5 Diagnosis
- 6 Treatment
- 7 References
Characteristics
General characteristics and growing conditions
Serratia marcescens it is a facultative aerobic bacillus, mobile like most Enterobacteriaceae. It is a ubiquitous inhabitant of soil, water, and the surface of plants. For this reason, it is common to find it in humid environments such as bathrooms, drains, sinks, sinks, etc..
It is able to survive under adverse conditions. For example, it can grow at temperatures from 3.5 ° C to 40 ° C. In addition, it can survive in soapy chlorhexidine solutions up to a concentration of 20 mg / mL..
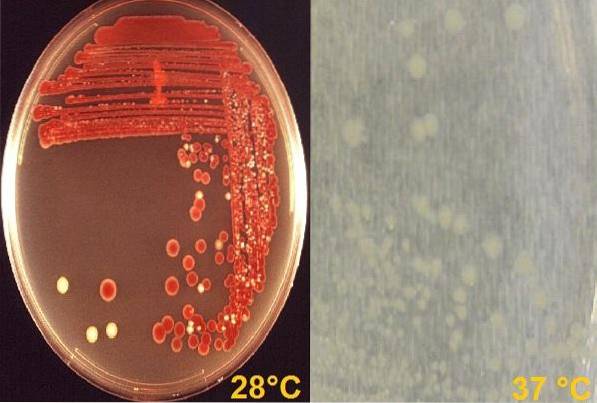
In the laboratory it can grow at room temperature (28 ° C), where some species develop a characteristic pigment of the brick-red color, called prodigiosin. But it also grows at 37 ° C, where its colonies are creamy white, that is, at this temperature it does not produce pigment..
This represents a temperature-stimulated physiological phenotypic variation. This characteristic is unique in this bacterium, as no other species of the family is capable of doing it..
Pigment production is undoubtedly a very useful tool for making the diagnosis..
In relation to the pH range that it can withstand, it ranges from 5 to 9.
Biochemical characteristics
Biochemically speaking Serratia marcescens complies with the basic characteristics that describe the entire Enterobacteriaceae family, that is, it ferments glucose, reduces nitrates to nitrites and is oxidase negative.
However, it has other biochemical characteristics that are described below:
S. marcescens tests positive for the following tests: Voges-Proskauer, citrate, motility, Lysine decarboxylase, ornithine and O-nitrophenyl-ß D-galactopyranoside (ONPG) and catalase.
While negative for: production of hydrogen sulfide (HtwoS), indole, phenylalanine deaminase, urea, and arginine.
Versus the methyl red test can be variable (positive or negative).
Finally, compared to kligler medium, it produces an alkaline / acid reaction, that is, it ferments glucose with gas production but not lactose.
Virulence factors
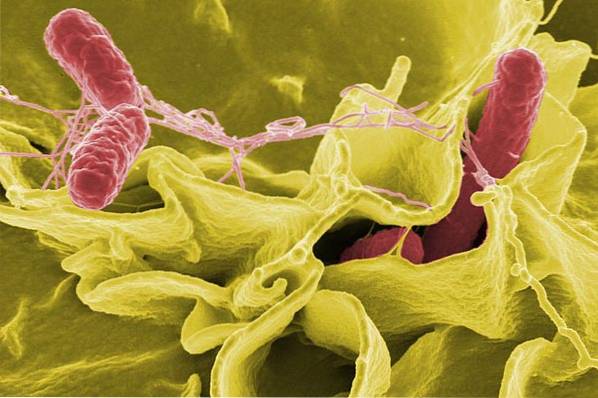
The genus Serratia stands out within this family for having 3 important hydrolytic enzymes: lipase, gelatinase and extracellular DNase. These enzymes favor the invasiveness of this microorganism.
It also has 3 chitinases and a chitin-binding protein. These properties are important in the degradation of chitin in the environment.
Also, kinases provide the property to S. marcescens to exert an anti-fungal effect on Zygomycete fungi, whose cell wall is mainly composed of chitin.
On the other hand, S. marcescens it is capable of forming biofilms. This represents an important virulence factor, since in this state the bacterium is more resistant to the attack of antibiotics..
Recently it has been found that some strains of S. marcescens They present a type VI secretion system (T6SS), which is used for the secretion of proteins. However, its role in virulence has not yet been defined..
Antimicrobial resistance
Strains of S. marcescens Chromosomal Betalactamase-producing AmpC type.
This gives them an intrinsic resistance to ampicillin, amoxicillin, cefoxitin and cephalothin, with which the only option among Beta-lactams for the treatment of ESBL-producing strains would be carbapenems and piperacillin tazobactam..
Additionally, it has the ability to acquire resistance mechanisms to other commonly used antibiotics, including aminoglycosides..
Strains of S. marcescens producing KPC-2 and bla TEM-1. In this case, carbapenems are no longer efficient..
The first KPC strain outside the hospital setting was isolated in Brazil, being resistant to aztreonam, cefepime, cefotaxime, imipenem, meropenem, gentamicin, ciprofloxacin and cefazidime, and only susceptible to amikacin, tigecycline and gatifloxacin.
Taxonomy
Dominium: Bacteria
Phylum: Proteobacteria
Class: Gamma Proteobacteria
Order: Enterobacteriales
Family: Enterobacteriaceae
Tribe: Klebsielleae
Genus: Serratia
Species: marcescens.
Morphology
They are long bacilli that turn red against Gram staining, that is, they are Gram negative. It does not form spores. They have peritric flagella and lipopolysaccharide in their cell wall.
Pathologies and symptoms
Among the pathologies that can cause Serratia marcescens in debilitated patients are: urinary tract infection, wound infection, arthritis, conjunctivitis, endophthalmitis, keratoconjunctivitis and ulcerative keratitis.
Likewise, it can cause more serious pathologies such as: septicemia, meningitis, pneumonia, osteomyelitis and endocarditis.
The entry point for these pathologies is usually represented by contaminated solutions, venous catheters with biofilm formation or other contaminated instruments..
In the case of ophthalmic pathologies, it is mainly caused by the use of contact lenses colonized with this or other bacteria. In this sense, ulcerative keratitis is the most serious ophthalmic complication, which occurs in contact lens wearers. It is characterized by loss of epithelium and stromal infiltration, which can lead to loss of vision.
Another less aggressive ophthalmic manifestation is that of CLARE syndrome (contact lens-induced acute red eye). This syndrome manifests with acute pain, photophobia, tearing and redness of the conjunctiva without epithelial damage..
Diagnosis
They grow on simple media such as nutrient agar and brain heart infusion, on enriched media such as blood agar and chocolate.
In these media, the colonies tend to turn creamy white if incubated at 37 ° C, while at room temperature the colonies may present a red-orange pigment..
They also grow on MacConkey agar selective and differential medium. In this case, the colonies grow pale pinkish or colorless at 37 ° C and at 28 ° C their color tone increases..
Müeller Hinton agar is used to perform the antibiogram..
Treatment
Due to the natural resistance of this bacterium to first-generation penicillins and cephalosporins, other antibiotics should be used as long as they are sensitive in the antibiogram and there are no resistance mechanisms such as the production of extended-spectrum beta-lactamases, among others..
Among the antibiotics that can be tested for susceptibility are:
- Fluorquinolones (ciprofloxaz or lebofloxacin),
- Carbapenems (ertapenem, imipenem, and meropenem),
- Third-generation cephalosporins (cefotaxime, ceftriaxone, or cefadroxil),
- Fourth generation cephalosporin (cefepime),
- Aminoglycosides (amikacin, gentamicin, and tobramycin),
- Chloramphenicol is especially useful in cases of infections where the formation of biofilms is involved..
References
- Hume E, Willcox M. Appearance of Serratia marcescens as an ocular surface pathogen. Arch Soc Esp Oftalmol. 2004; 79 (10): 475-481
- Ryan KJ, Ray C. Sherris. Microbiology Medical, 2010. 6th Ed. McGraw-Hill, New York, U.S.A
- Koneman, E, Allen, S, Janda, W, Schreckenberger, P, Winn, W. (2004). Microbiological Diagnosis. (5th ed.). Argentina, Editorial Panamericana S.A.
- Hover T, Maya T, Ron S, Sandovsky H, Shadkchan Y, Kijner N. Mitiagin Y et al. Mechanisms of bacterial (Serratia marcescens) Attachment to, migration along, and killing of fungal Hyphae. Appl Environ Microbiol. 2016; 82 (9): 2585-2594.
- Wikipedia contributors. Serratia marcescens. Wikipedia, The Free Encyclopedia. August 14, 2018, 16:00 UTC. Taken from wikipedia.org.
- Sandrea-Toledo L, Paz-Montes A, Piña-Reyes E, Perozo-Mena A. Extended spectrum ß-lactamase-producing enterobacteria isolated from blood cultures in a University Hospital of Venezuela. Kasmera. 2007; 35 (1): 15-25. Available at: Scielo.org
- Murdoch S, Trunk K, English G, Fritsch M, Pourkarimi E, and Coulthurst S. The Opportunistic Pathogen Serratia marcescens Utilizes Type VI Secretion To Target Bacterial Competitors. Journal of Bacteriology. 2011; 193(21): 6057-6069.
- Margate E, Magalhães V, Fehlberg l, Gales A, and Lopes. Kpc-producing Serratia marcescens in a home-care patient from recife, Brazil. Journal of the Institute of Tropical Medicine of São Paulo, 2015; 57(4), 359-360.


Yet No Comments