
Gate theory How do we perceive pain?
The gate theory highlights the importance of the brain in the perception of pain, basically consisting in the fact that the presence of a non-painful stimulus blocks or reduces a painful sensation.
Pain is not pleasant, but it is necessary for our survival. It works by warning the individual that there is a danger to their body or their health, with the aim of interrupting the cause of that pain to maintain the integrity of the body.

For example, pain is what causes you to remove your hand from the fire if you are burning, or to hold a part of your body still to recover through rest. If we did not feel pain, we could do ourselves serious harm without realizing it.
However, there are times when the pain is not adaptive, such as in a surgical intervention or in childbirth, for example..
As it may happen to us that the sensation of pain may seem more or less intense depending on various factors, such as the cognitive interpretation we give it: the pain you feel if someone has intentionally hurt you is not the same as the pain you feel when you have been stepped on or pushed by accident.
Therefore, this shows that pain can be something subjective and multidimensional, since many parts of the brain participate in building it, containing the following aspects: cognitive, sensitive, affective and evaluative.
This theory was developed in 1965 by Ronald Melzack and Patrick Wall. It is the most revolutionary contribution to the understanding of pain mechanisms, based on neural mechanisms. This led to the acceptance that the brain is an active system that selects, filters and transforms stimuli from the environment.
When this theory was proposed, it was met with great skepticism. However, most of its components are still in use today.
Article index
- 1 Systems involved in gate theory
- 1.1 Peripheral nervous system
- 1.2 Central nervous system
- 2 Previous theories
- 2.1 Theory of specificity
- 2.2 Theory of intensity
- 3 How is the mechanism of the gate theory?
- 3.1 Brain nerve impulses
- 4 Why do we rub our skin after a blow?
- 4.1 Methods that relieve pain
- 5 Factors Influencing Gate Theory
- 6 References
Systems involved in gate theory
The gate theory provides a physiologically based explanation for pain processing. To do this, you have to focus on the complex functioning of the nervous system, which contains two main divisions:
Peripheral nervous system
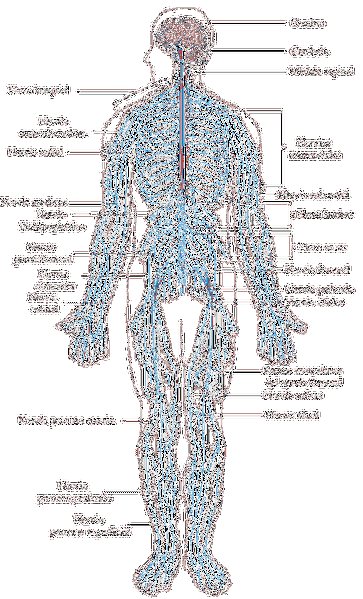
They are the nerve fibers that exist in our body, outside the brain and spinal cord, and include nerves in the lumbar spine, in the torso and the extremities. The sensory nerves are those that carry information about heat, cold, pressure, vibration and of course, pain to the spinal cord from different parts of the body..
Central Nervous System

Covers the spinal cord and brain.
According to the theory, the experience of pain will depend on the functioning and interaction of these two systems.
Previous theories
Specificity theory
After damage to our body, pain signals appear in the nerves surrounding the damaged area, traveling to the peripheral nerves to the spinal cord or brain stem, and then to our brain, which will make sense of that information..
This would correspond to a theory prior to the gate theory, called the specificity theory of pain. This theory defends that there are specialized pathways for each somatosensory modality. Thus, each modality has a specific receptor and is linked to a sensory fiber that responds to a specific stimulus..
As Moayedi and Davis (2013) explain, these ideas have emerged over thousands of years and were finally demonstrated experimentally, officially being considered as a theory in the 19th century by Western European physiologists..
Intensity theory
This theory has been postulated at different times in history, being able to establish Plato as its precursor; since he considered pain as the emotion that arises after a more intense stimulus than normal.
Little by little and through different authors in history, it has been concluded that pain seems to be associated with a summative effect of stimuli: repeated stimulation, even if it is of little intense stimuli as well as a very intense stimulation that passes the threshold, produces pain.
Goldscheider was the one who defined the neurophysiological mechanisms to describe this theory, adding that this summation was reflected in the gray matter of the spinal cord..
- Peripheral pattern theory: This theory differs from the previous two, and was developed by J.P. Nafe (1929), stating that any somatosensory sensation is produced by a particular pattern of neuronal firing. In addition, the activation patterns of spatial and temporal neurons would determine what type of stimulus it is and how intense it is..
The gate theory collects different ideas from these previous theories of pain perception and adds new elements that we will see below..
How is the mechanism of the gate theory?
The gate theory proposes that, when we injure ourselves or hit any part of the body ...
-Two types of nerve fibers are involved in perception: fine or small diameter nerve fibers, which are responsible for transmitting pain (called nociceptive) and which are not myelinated; and large or myelinated nerve fibers, which participate in the transmission of tactile, pressure or vibratory information; and that they are not harmful.
Although if we classify them as nociceptive or non-nociceptive, the so-called “A-Delta” nerve fibers and “C” fibers would enter the first group, while those that do not transmit pain are the “A-Beta”.
- Dorsal horn of the spinal cord: The information carried by these two types of nerve fibers will reach two places in the dorsal horn of the spinal cord: the transmitter cells or T cells of the spine, which are those that transmit pain signals to the central nervous system; and inhibitory interneurons whose task is to block the actions of T cells (i.e., block the transmission of pain).
- Each fiber has a function: In this way, the fine or large nerve fibers activate the transmitter cells that will transport the information to our brain to interpret it. However, each type of nerve fiber has a different function in perception:
- The fine nerve fibers they block inhibitory cells, and therefore by not inhibiting, allow pain to spread; what is defined as "opening the door".
- However, thick nerve fibers Myelinated cells activate inhibitory cells, causing pain transmission to be suppressed. This is called "closing the gate.".
In short, the more activity the large fibers have compared to the fine fibers on the inhibitory cell, the less pain the person will perceive. So the different activity of the nerve fibers will compete to close or open the gate.
On the other hand, when a certain critical level of activity of the fine or small-diameter fibers is reached, a complex action system is activated that manifests itself as an experience of pain, with its typical behavior patterns such as withdrawal or withdrawal from the painful stimulus..
Brain nerve impulses

In addition, the spinal mechanism is influenced by nerve impulses that arrive from the brain. In fact, there is an area of the brain that is responsible for reducing the sensation of pain, and it is the periaqueductal or central gray matter, which is located around the cerebral aqueduct of the midbrain.
When this area is activated, the pain disappears by having consequences in the pathways that block the nociceptive nerve fibers that reach the spinal cord..
On the other hand, this mechanism can occur by a direct process, that is, from the place where the damage has occurred directly to the brain. It is produced by a type of thick and myelinated nerve fibers, which rapidly transmits information of severe pain to the brain.
They differ from non-myelinated fine fibers in that the latter transmit pain more slowly and in a much longer way. In addition, opioid receptors in the spinal cord are also activated, associated with analgesia, sedation and well-being..
Thus, little by little our brain determines which stimuli to ignore, it will regulate the perceived pain, adjust its meaning, etc. Since, thanks to brain plasticity, the perception of pain is something that can be modeled and exercised to reduce its effects when they are not adaptive for the person.
Why do we rub our skin after a blow?
The gate theory can offer us an explanation of why we rub an area of the body after having received a blow to it.
It seems that, after an injury, the mechanisms already described are triggered, producing an experience of pain; but when you rub the affected area you start to feel relief. This occurs because large, fast nerve fibers called A-Beta are activated..
These send information about touch and pressure, and are responsible for activating interneurons that eliminate pain signals transmitted by other nerve fibers. This happens because when the spinal cord is activated the messages go directly to various brain areas such as the thalamus, the midbrain and the reticular formation..
In addition, some of these parts involved in receiving pain sensations also participate in emotion and perception. And, as we said, there are areas like the periaqueductal gray matter and the nucleus magnus of the raphe, which connect to the spinal cord again changing the information present and thereby reducing pain..
Methods that relieve pain
Now it seems to make sense why massage, heat, cold compresses, acupuncture, or transcutaneous electrical stimulation (TENS) can be pain-relieving methods..
The latter method is based on the gate theory and is one of the most advanced instruments for pain management. Its function is to electrically and selectively stimulate large diameter nerve fibers that cancel or reduce pain signals.
It is widely used to alleviate chronic pain that does not improve with other techniques such as fibromyalgia, diabetic neuropathy, cancer pain, etc. It is a non-invasive method, low cost and without secondary symptoms such as drugs can have. However, there are doubts about its long-term efficacy and there are cases in which it does not seem to be effective..
It appears, then, that the gate theory does not contemplate all the complexity that the underlying mechanisms of pain actually represent. Although it has contributed in an important way to develop pain management strategies.
New research is currently being published that adds new components to this theory, refining its mechanism..
Factors influencing the gate theory
There are certain factors that will determine the conception of pain signals regarding the opening or closing of the gate (whether the pain reaches the brain or not). These are:
- The intensity of the pain signal. This would have an adaptive and survival purpose, because if the pain is very strong it would warn of a great danger to the individual's body. So this pain is difficult to alleviate by the activation of non-nociceptive fibers.
- The intensity of other sensory signals such as temperature, touch or pressure if they occur in the same place of damage. That is, if these signals exist and are intense enough, the pain will be perceived in a lighter way as the other signals gain in intensity..
- The message from the brain by itself (to send signals that pain is occurring or not). This is modulated by previous experience, cognitions, mood, etc..
References
- Deardorff, W. (March 11, 2003). Modern Ideas: The Gate Control Theory of Chronic Pain. Obtained from Spine-health
- Gate Control Theory. (s.f.). Retrieved on July 22, 2016, from Wikipedia
- Hadjistavropoulos, T. & Craig, K.D. (2004). Pain: Psychological Perspectives. Psychology Press, Taylor & Francis Group: New York.
- Moayedi, M., & Davis, K. (n.d). Theories of pain: from specificity to gate control. Journal Of Neurophysiology, 109 (1), 5-12.
- Pain and Why It Hurts. (s.f.). Retrieved on July 22, 2016, from the University of Washington
- The gate control theory of pain. (1978). British Medical Journal, 2 (6137), 586-587.
- Wlassoff, V. (June 23, 2014). Gate Control Theory and Pain Management. Obtained from BrainBlogger



Yet No Comments