
Windpipe

What is the trachea?
The windpipe it is a flexible cylindrical duct about 12-14 cm long in adult humans, and about 2 cm in diameter. It begins in the cricoid cartilage of the larynx and ends up bifurcating (dividing in two, like a "Y") and giving rise to the right main bronchus and the left main bronchus..
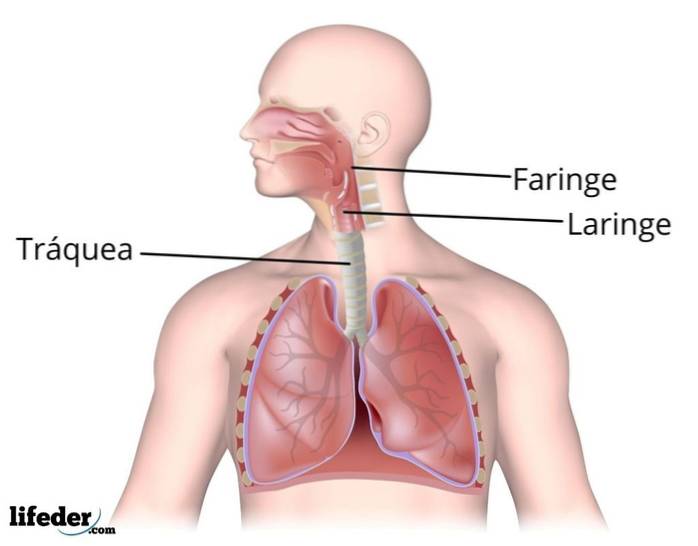
This structure is part of the air conduction system of the respiratory system of man and many other vertebrate animals. Anatomically, the trachea is located between the larynx and the main bronchus of each lung (right and left).
The air conduction system of the human respiratory system is made up of the nasal passages and nasal cavity, the paranasal sinuses, the pharynx (common passage for food and air), the larynx (which contains the vocal cords), the trachea , the bronchi and the structure of pulmonary tubes and ducts.
Characteristics of the trachea
The trachea is a tube whose posterior part is flattened and extends from the lower part of the larynx to the level of the fourth dorsal vertebra, where it bifurcates giving rise to the two main bronchi.
Histologically speaking, it is made up of three different tissue layers, known as the mucosa, submucosa, and adventitia..
The cells present in these layers participate in the conduction of air and in the secretion of mucus and the elimination of foreign substances from the respiratory tract..
Respiration consists of two phases: inspiration or air entry and expiration or air exit. During inspiration, the trachea widens in diameter and increases in length, while during expiration it returns to its normal condition, that is, it returns to the initial condition prior to inspiration..
Functions of the trachea
Air conduction
The main function of the trachea is to conduct air from the environment, which reaches through the nostrils and larynx, to the main bronchi and subsequently to the lungs..
Defense of the organism
Another important function of this portion of the respiratory tract is to eliminate, through the ciliary sweep of mucus, foreign substances or suspended particles that enter with the air, preventing them from reaching the most sensitive or delicate parts of the lung, that is, to the pulmonary alveoli, which represent the main sites of gas exchange.
The trachea reacts to irritating substances by contracting the smooth muscles associated with it, triggering the cough reflex.
The contraction of these muscles reduces the diameter of the trachea and, together with the violent contraction of the expiratory muscles and the abrupt opening of the glottis, helps to increase the speed of air flow and the elimination of irritating substances..
Thermoregulation
Along with the nasal passages and sinuses, the trachea participates in the heating and humidification (saturation of water vapor) of the air entering the respiratory tract..
Parts and histology
The trachea is made up of three layers of tissue, which are:
- Mucosa
- The submucosa
- Adventitia
Much of the trachea is outside the chest, in the front of the neck, and in front of the esophagus. Then it enters the internal part of the thorax (mediastinum), located behind the sternum, until it reaches the level of the fourth dorsal vertebra, where it bifurcates.
Adventitial layer of trachea
This is the outermost layer of the trachea, it is made up of fibroelastic connective tissue, hyaline cartilage and fibrous connective tissue. It works in fixing the trachea to adjacent structures such as the esophagus and connective tissues of the neck.
The adventitial layer is where the tracheal rings are located, which are more than a dozen, and which are made up of hyaline cartilage. Said rings are shaped like a "C" or horseshoe; the “open” part of the horseshoe is directed towards the back of the windpipe, that is, as if looking towards the dorsal part of the body.
Between each cartilaginous ring is a layer of intermediate fibrous connective tissue. Each ring, at its back, joins the next through a layer of smooth muscle known as the tracheal muscle. The contraction of this muscle reduces the diameter of the trachea and increases the speed of flow and the evacuation of foreign substances..
The arrangement of the rings and the tracheal muscle make the posterior part of the trachea flat and the anterior part rounded.
Just above where the bifurcation of the trachea occurs, the cartilaginous rings come together to completely surround the airway. The muscular covering of the muscular part of the trachea is reorganized forming a separate layer of interlaced fascicles within said cartilages..
Submucosal layer of the trachea
The submucosal layer contains mucous and seromucosal glands embedded in dense and irregular fibroelastic tissue. It is located spatially between the mucous layer and the adventitia and is rich in blood and lymphatic vessels.
The ducts of the glands in this layer are short and pierce the lamina propria of the epithelium, draining their products towards the inner surface of the trachea..
Mucous layer of the trachea
It is the layer that covers the inner portion of the trachea (covering layer) and is separated from the submucosa by a bundle of fairly thick elastic fibers. It is composed of a respiratory epithelium (ciliated pseudostratified epithelium) and a lamina propria of subepithelial connective tissue.
The respiratory epithelium
It is made up of several types of cells, including goblet cells, ciliated cylindrical cells, other brush cells, basal cells, serous cells and cells of the diffuse neuroendocrine system..
All of these cells reach the basement membrane, but not all reach the lumen of the trachea (the internal space of the duct). The most abundant are ciliated columnar cells, goblet cells, and basal cells..
- The cylindrical ciliated cells, As their name indicates, they are cells with an apical plasma membrane differentiated into cilia and microvilli, whose movement is upward, that is, from the bottom to the top or towards the nasopharyngeal tract..
The main function of these cells is to "facilitate" the movement of the mucus and the particles contained in it out of the trachea..
- The goblet cells are responsible for the production of mucinogen, which is one of the main components of mucus and, in the respiratory system, these are cells with a narrow base and an expanded upper part, rich in secretory granules loaded with mucin.
- The basal cells they are short in length and are attached to the basement membrane, but do not reach the luminal surface of the mucosa. Stem cells are considered for the regeneration of goblet cells, hair cells and brush cells.
- The serous cells they are the least abundant in the tracheal mucosa. They are cylindrical cells that have microvilli and apical granules loaded with the electrodense serous fluid that they secrete..
- The brush cells, as well as serous cells, they are found in a very low proportion. They also have high microvilli and some researchers suggest that they may have sensory functions, as they have been linked to nerve endings..
- The cells of the diffuse neuroendocrine system, also known as "small granule cells", they are rare in the mucosa. These contain granules that are apparently released into the connective tissue spaces of the lamina propria, secretions that appear to control the functions of other cells of the respiratory epithelium..
The lamina propria
This layer is made up of loose fibroelastic connective tissue and contains lymphoid tissues such as lymph nodes, lymphocytes, and also neutrophils. Some seromucosal glands and mucus are also found in the lamina propria..
Diseases
Like all organic tissue, the trachea is susceptible to certain conformational alterations caused by congenital problems, by infections and benign or malignant tumors and by alterations in its structure due to the continuous inhalation of irritants.
Tracheal metaplasia
One of the most frequent alterations of the trachea is tracheal metaplasia, which consists of a reduction in the number of hair cells in the mucous layer and an increase in mucus-producing goblet cells, typical of chronic cigarette smoking or recurrent exposure to coal dust.
The increase in the number of goblet cells increases the thickness of the mucus layer, but the decrease in the number of ciliated cells reduces their elimination from the tracheal tube, resulting in chronic congestion of the airways and lungs..
Tracheoesophageal fistulas
Among the congenital alterations of the trachea, it is worth mentioning the tracheoesophageal fistulas, which are abnormal tubes that connect the trachea with the esophagus; tracheal stenosis (a congenital reduction in the diameter of the trachea); cartilage agenesis (absence of tracheal cartilage that causes the collapse and closure of the trachea), among others.
Infections or tumors
Other tracheal pathologies have to do with infections of viral or bacterial origin, or the development of benign or carcinomatous tumors..
Other
Finally, there are alterations associated with retractable scars that occur in the trachea due to penetrating injuries or tracheostomy, an intervention in which a tube is placed inside the trachea to connect patients who require assisted respiration for very long periods of time..
These scars produce local narrowing of the trachea that can cause difficulty in breathing and that must be treated surgically..
References
- Ganong, W. F. (1980). Manual of Medical Physiology.
- Gartner, L. P., & Hiatt, J. L. (2006). Color textbook of histology ebook. Elsevier Health Sciences.
- Johnson, K. (1991). Histology and Cell Biology (2nd ed.). Baltimore, Maryland: The National medical series for independent study.
- Netter, F. H., & Colacino, S. (1989). Atlas of human anatomy. Ciba-Geigy Corporation.
- Ross, M., & Pawlina, W. (2006). Histology. A Text and Atlas with correlated cell and molecular biology (5th ed.). Lippincott Williams & Wilkins.



Yet No Comments