
Basilica vein
What is the basilica vein?
The basilica vein It is a vein belonging to the superficial venous drainage system of the upper limb. Its birth and trajectory are relatively variable and its pathologies are rare. Etymologically, its name comes from the Greek that sounds basiliké, which means "royal" or "proper of kings".
Semantically, this Greek term evolved to acquire various meanings, among them that of "the most important", meaning coined in Galenic medicine in view of the fact that the basilic vein was treated as the most important vessel for performing phlebotomies and bloodletting. upper limb.
In its constitution, the venous system of the arm has two components: a superficial venous system (to which the basilic vein belongs) and a deep venous system. Knowledge of the tributaries, function and anatomy of the basilic vein is of great importance today.
This is so because it allows, among other things, the determination of some vascular pathologies of the upper limb. In addition, this vein represents an option for vascular access in patients with hemodialysis requirements..
Path of the basilica vein
Although there is a lot of variability with respect to the origin of this venous vessel, the most widely accepted route and relationships are those described below:
Forearm portion
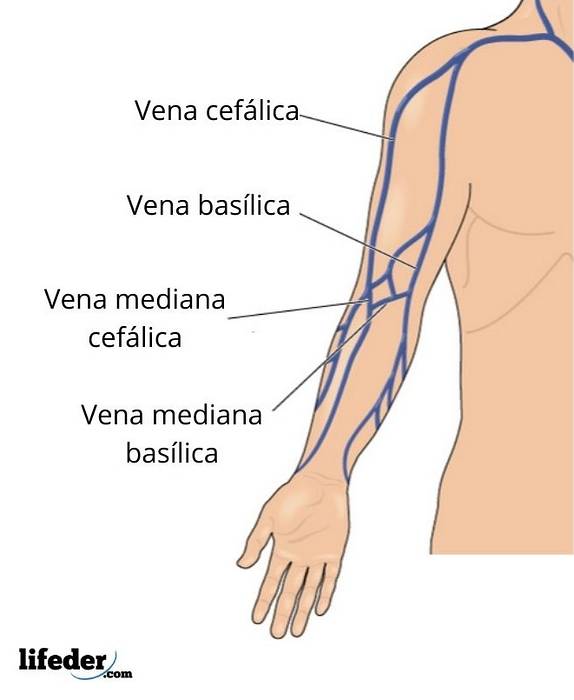
The basilic vein begins its journey in the ulnar or ulnar (medial) portion of the dorsal venous network of the hand. After a short journey on its posterior surface, it leans forward to travel almost always superficially and above fascies and muscles on the medial side of the forearm..
It is at this point that it acquires the name of the basilic vein of the forearm. Upon reaching the elbow joint, it is located on the anterior surface, just below it..
Brachial portion
It goes up the inner channel of the elbow; after this it ascends obliquely between the biceps brachii and pronator teres muscles to later cross the brachial artery, from which it is separated by the fibrous lacertus (fibrous sheet that separates the artery from the vein).
Filaments of the medial cutaneous nerve of the forearm run in front of and behind this portion of the basilic vein.
Finally, it ends its journey by traversing the medial border of the biceps brachii muscle, piercing the deep fascia slightly below the middle of the arm, and then ascending the medial side of the brachial artery, until it reaches the lower border of the teres major muscle in where it continues as a tributary of the internal humeral vein.
Tributaries, anastomosis, and variability
Among the known variations corresponding to the anatomy of the basilic vein, the following are some of the most accepted:
- Sometimes it may flow into or be a tributary of the axillary vein instead of ending in the internal humeral vein.
- The antebrachial portion of the basilic vein may have an anastomosis with the deep radial veins.
- The brachial portion of the basilic vein may have an anastomosis with the cephalic vein in the arm. The most commonly known anastomosis is the median ulnar vein..
- The posterior and anterior circumflex humeral veins can join the basilic vein as tributaries at the precise moment before the latter meets the humeral veins to generate the axillary vein..
Function of the basilic vein
The basilic vein, as well as the set of veins belonging to the superficial venous drainage system of the upper limb, shows as its main characteristic that it comprises vessels of greater volumetric capacity.
As it is in communication with the veins that run along the lateral part of the upper limb and, in turn, because it runs all over the upper limb, it is impossible to separate the function of the basilic vein in a segmental way..
Only its physiological role as a blood drainage vessel of the arm can be described, which acts in conjunction with the other components of the superficial venous system of the upper limb..
Posible problems
Among some of the pathologies in which the basilic vein may be compromised, it is necessary to take into account trauma involving the limb, puncture phlebitis, hypercoagulable states and endothelial damage that condition venous stasis (conditions of Virchow's triad) and cause venous thrombosis pictures.
Venous thrombosis of the upper limb is quite rare, unlike deep vein thrombosis of the lower limb; However, a related entity known as Paget-Schrotter syndrome, also called thoracic or cervicothoracic outlet syndrome, has been described..
This syndrome is categorized into 3 subgroups, depending on the structures that are compressed; In this case, venous compression is of particular interest, corresponding to the most common of the vascular subgroups above the arterial one, and is seen in 3 to 4% of cases with this syndrome.
It consists of a thrombosis that may well be both primary and secondary; This condition is also known as stress thrombosis. This syndrome was described by Paget in 1875; and by Schrötter, in the year 1884.
Its pathophysiology includes compression of those veins located under the pectoralis minor and the diagnostic method of choice is performed by venography.
Regarding its clinical manifestations, the signs and symptoms come to view 24 hours after the thrombosis with edema, dilation of the collateral veins, discoloration and continuous pain.
Eventually, the upper limb becomes cold and the patient reports difficulty in mobility of the fingers. It is important to note that the distention of the venous system is especially noticeable in the basilic and cephalic veins..
The treatment of choice for this syndrome at present is fibrinolytics, which, initiated between the first 3 to 5 days after the onset of the clinical picture, have been shown to be 100% effective..
References
- Falconer MA, Weddell G: Costoclavicular compression of the subclavian artery and vein: relation to the scalenus anticus syndrome. Lancet 1943; 2: 539.
- Drake R.L., Vogl A., Mitchell, A.W.M. GRAY. Anatomy for students + Student Consult. 2011. Elsevier. Madrid.
- Liñares S. [Internet]. Circulatory system. Recovered from: anatomia-vascular.blogspot.com.es
- Peivandi MT, Nazemian Z. Clavicular fracture and upper-extremity deep venous thrombosis. Orthopedics. 2011; 34 (3): 227.
- Basilica vein of the forearm. Recovered at: imaios.com



Yet No Comments