
Tubular adenoma symptoms, causes, types, treatments
The tubular adenoma it is the most common type of polyp in the colon (large intestine). It is estimated that it affects between 20 and 30% of people over 50 years of age. It is a benign lesion with the potential for malignancy, so once they are identified it is necessary to remove it in order to eliminate the risk of colon cancer development..
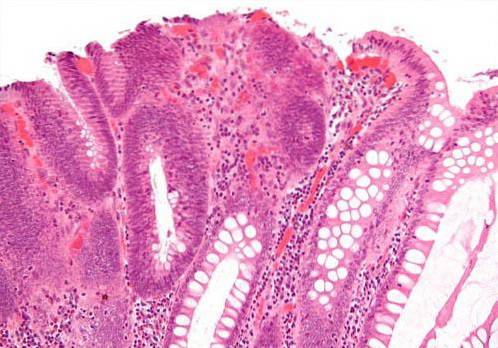
From a microscopic point of view, tubular adenomas are made up of well-organized epithelial tubules, which in turn are made up of cells with “different” characteristics from normal colon cells, hence this type of polyp is considered dysplasia. low grade.
Regular screening is recommended for both polyps (including tubular adenoma) and colon cancer, since when diagnosed early, the prognosis is usually excellent..
Article index
- 1 Symptoms
- 2 Causes
- 3 Types
- 3.1 Pedunculated tubular adenomas
- 3.2 Sessile tubular adenomas
- 3.3 Kudo classification
- 4 Diagnosis
- 5 Treatments
- 6 References
Symptoms
90% of tubular adenomas are asymptomatic; a patient may have one or multiple and feel absolutely nothing. When symptoms do occur (10% of cases), they are usually nonspecific and attributable to multiple causes..
Of the potential symptoms, the most frequent is lower gastrointestinal bleeding, which in most cases is microscopic; This means that the patient does not notice anything, being necessary the study of occult blood in feces to be able to identify the hemorrhage.
In rare cases, the hemorrhage is large enough that the stool shows blood detectable by direct inspection; When this occurs, they are usually very large tubular adenomas that have evolved for several years, with the risk of malignancy being much higher in these cases..
Another of the symptoms that can occur are changes in the intestinal pattern (quantity, quality and type of evacuations), presenting in many cases diarrhea, although when a tubular adenoma is large enough it can partially obstruct the lumen of the large intestine generating constipation.
Likewise, there may be a change in the morphology of the stool, especially when the adenoma is located in the rectum and is large. In these cases, the stool becomes narrower than normal, this evacuation pattern being known as “tapered stool” (stool that looks like a ribbon).
On rare occasions abdominal pain or rectal prolapse of the tubular adenoma may occur, with very few cases reported in the literature in this regard.
Causes
There is no known single and definite cause of tubular adenomas (as well as of any other type of colon polyp), however there are risk factors that increase the chances of presenting this condition.
Of all the risk factors for tubular adenoma, the most important is the genetic factor. The activation or inactivation of certain groups of genes cause colon cells to grow in a disorderly way and begin to form adenomas or other types of polyps in the first instance, later developing colon cancer.
Since the genetic factor is so significant, the fact that a person has a blood relative in the first degree (father, mother, brother, son) who has or has presented colon tubular adenoma, significantly increases the risk that that person also the present, in fact there is a very well established hereditary-family pattern.
However, not all tubular adenomas present in the context of a patient with a family history of tubular adenoma; In these cases, other risk factors such as excessive alcohol consumption, tobacco use (smoking), obesity and sedentary lifestyle must be considered..
In addition, patients with inflammatory diseases of the colon (ulcerative colitis, Chron's disease) are more likely to develop any type of colon polyp, including tubular adenomas..
Types
From the macroscopic point of view, tubular adenomas can be classified into two large groups according to their morphological characteristics; Pedunculated tubular adenomas and sessile tubular adenomas.
Both types can be divided into two large groups according to their size: tubular adenomas smaller than 1 cm and tubular adenomas larger than 1 cm.
Regardless of the type (pedunculated or sessile), tubular adenomas smaller than 1 cm are considered to have a low risk of malignancy, while tubular adenomas larger than 1 cm are more likely to develop colon cancer.
On the other hand, tubular adenomas can be classified according to their microscopic characteristics according to the Kudo classification.
Pedunculated tubular adenomas
Pedunculated tubular adenomas are those that connect to the mucosa of the colon through a “foot” or “pedicle”. They resemble a mushroom whose narrow part (foot) is connected to the mucosa of the colon, while the wide part (polyp) is free in the lumen of the intestine connected to it only by the foot..
Sessile tubular adenomas
Sessile tubular adenomas are those that are attached to the mucosa of the colon throughout its base. They resemble small domes that are attached to the mucosa of the large intestine, reaching considerable dimensions equal to or greater than 5 cm.
Kudo classification
The Kudo classification divides tubular adenomas into five different categories according to the glandular pattern observed on endoscopic magnification..
This classification is applicable not only to tubular adenomas, but to any other colon polyp (villous adenoma, tubulo-villous adenoma). The five categories of the Kudo classification are:
I. Normal Crypt Pattern, with unbranched glands and with circular orifices arranged at regular intervals.
II. Cross or star shaped pattern, larger than normal, typical in hyperplastic polyps.
IIIL. Long tubular, curves, present in adenomatous lesions, dysplasia present.
IIIs. Small tubular or circular, Small, compactly arranged crypts, typical of depressed lesions, often associated with high-grade dysplasia or carcinoma in situ.
IV. Cerebriform appearance, combine branched neoplastic glands with long, tortuous crypts, common in lesions with a hairy component.
V. Irregular intramucosal, disorganized, unstructured glands surrounded by adenomatous and inflammatory tissue suggesting invasion. Submucosal carcinoma.
Diagnosis
There are various methods for the investigation and diagnosis of tubular adenomas, some more sensitive and specific than others..
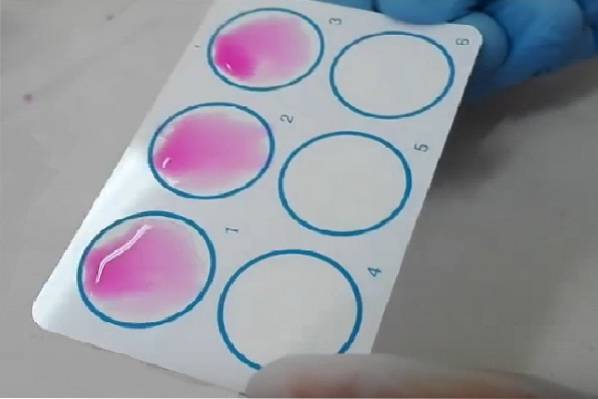
For many years the use of fecal occult blood has been advocated as a screening method, both for tubular adenoma and for other polyps and even malignant colon lesions, however this test is useful only if the adenoma bleeds, in otherwise it has no diagnostic value.
For its part, flexible colonoscopy, even when it is more invasive, is much more useful for the diagnosis of tubular adenomas (as well as for any other colon lesion), since it allows not only to visualize the macroscopic characteristics of the polyps, but also perform biopsies for histological confirmation.
Biopsy itself can be considered the gold standard for the diagnosis of any colon polyp, including tubular adenoma, however with the advent of endoscopy with magnification and chromoendoscopy every day it is less frequent to perform biopsies to distinguish malignant lesions of benign lesions.
Since adenomas (including tubular adenoma) are the only polyps with the potential for long-term malignancy, endoscopic magnification techniques and chromoendoscopy have sought to develop the ability to distinguish adenomas from all other types of polyps, making so it is unnecessary to perform a biopsy in order to obtain a definitive diagnosis.
In addition, magnification and chromoendoscopy techniques allow the early diagnosis of tubular adenomas and other incipient colon lesions, which are too small to be detected by conventional colonoscopy. This makes it possible to diagnose tubular adenomas and other types of polyps very early, significantly improving the prognosis of the patient..
Treatments
Since 5% of tubular adenomas will degenerate into cancer (usually about 14-15 years after first appearance), removal is recommended whenever they are diagnosed, especially if the patient has a history of colon cancer.
The method of removal varies according to the number of polyps, the location, the patient's risk factors, and the size of the lesions..
In general, pedunculated small polyps in patients with few risk factors, endoscopic polypectomy can be performed, a procedure that can be performed under sedation in the office and whose success rates make it the procedure of choice whenever it is necessary. feasible to do it.
When the polyps are very large or very numerous as well as in those cases where there is intestinal obstruction, it will be necessary to perform surgery.
The type of surgery will largely depend on the location of the polyps.
When it comes to single polyps located in the lower rectum, it is possible to perform a transanal resection of them.
In those cases of multiple, large tubular adenomas or with signs of malignancy, it will be necessary to perform colon resection (colectomy), which can be partial (right or left hemicolectomy depending on the location of the lesions) or total (total colectomy).
In all cases where endoscopic polypeptomy is performed, as well as when partial colon resections are planned, endoscopic control will be necessary every 2 to 5 years since there is the possibility that new tubular adenomas (or other types of polyps) may develop through the long of the time.
References
- Noshirwani, K. C., Van Stolk, R. U., Rybicki, L. A., & Beck, G. J. (2000). Adenoma size and number are predictive of adenoma recurrence: implications for surveillance colonoscopy. Gastrointestinal endoscopy, 51(4), 433-437.
- Wolber, R. A., & Owen, D. A. (1991). Flat adenomas of the colon. Human pathology, 22(1), 70-74.
- Eberhart, C. E., Coffey, R. J., Radhika, A., Giardiello, F. M., Ferrenbach, S., & Dubois, R. N. (1994). Up-regulation of cyclooxygenase 2 gene expression in human colorectal adenomas and adenocarcinomas. Gastroenterology, 107(4), 1183-1188.
- Shinya, H. I. R. O. M. I., & Wolff, W. I. (1979). Morphology, anatomic distribution and cancer potential of colonic polyps. Annals of surgery, 190(6), 679.
- Gillespie, P. E., Chambers, T. J., Chan, K. W., Doronzo, F., Morson, B. C., & Williams, C. B. (1979). Colonic adenomas-a colonoscopy survey. Gut, twenty(3), 240-245.
- Levine, J. S., & Ahnen, D. J. (2006). Adenomatous polyps of the colon. New England Journal of Medicine, 355(24), 2551-2557.
- Lieberman, D. A., Weiss, D. G., Harford, W. V., Ahnen, D. J., Provenzale, D., Sontag, S. J. & Bond, J. H. (2007). Five-year colon surveillance after screening colonoscopy. Gastroenterology, 133(4), 1077-1085.


Yet No Comments