
Humoral immunity theory, effector mechanisms, examples

The humoral immunity, also known as the antibody-mediated immune response, it is one of the most important defense mechanisms of organisms against invasion by microorganisms or extracellular toxins.
Specifically, humoral immunity refers to immunity mediated by blood factors, which are serum proteins known as "antibodies" that function in responses to infections and are produced specifically in response to the presence of "antigens.".
The immune system of a mammal can be divided into innate immune system and adaptive immune system. The innate immune system consists of the different elements that function as physical and chemical barriers against the entry of invading agents into the body..
Among such barriers are the epithelia and some of the substances produced by them; some specific cell types are also involved, which together represent the body's first defense system.
The adaptive or specific immune system is a bit more complex and "evolved", since it is triggered in response to exposure to infectious agents or to contact with certain microorganisms, although both systems usually work together.
It is said to be a specific system because it occurs in response to defined determinants and is mediated by highly specialized cells that also have the ability to "remember" and respond more quickly and with more "strength" or "efficiency" to repeated exposures to same invading agent.
Humoral immunity is one of the subcategories of adaptive or specific immunity, which is also classified under cellular immunity. Both types of responses differ from each other depending on the component of the immune system involved..
Article index
- 1 Theory
- 1.1 A bit of history
- 2 Effector mechanisms
- 2.1 Phases of the humoral immune response
- 2.2 Lymphocytes and antibodies
- 2.3 Immunoglobulins
- 2.4 Humoral immune response
- 3 Examples
- 4 References
Theory
The theory of humoral immunity, which was the product of intense years of research and debate, proposes that immunity is mediated by substances present in body fluids or "humors.".
This theory was developed by many scientists, who independently studied and described many of the effectors involved in such response mechanisms..
Paul Ehrlich was perhaps one of the most influential, as he was the one who conducted the most in-depth studies on antigen-antibody complementarity in the early 1900s..
A little history
The renowned immunologist Rudolph Virchow, in 1858, established that all bodily pathologies were due to the malfunction of the cellular elements responsible for protection, rather than to a “mismatch of the soluble humors”.
Little more than 25 years later, in 1884, Eli Metchnikoff brought to light the first publication of the phagocytic theory, which today shapes and supports the main bases of the theory of cell-mediated immunity (cellular immunity)..
Many detractors of Metchnikoff tried to "disprove" his claims and it was in 1888 that George Nuttall, conducting a series of experiments designed to test Metchnikoff's theories, observed that the serum of normal animals had a "natural toxicity" against certain microorganisms.
In such a way, it became popular in the scientific world that cell-free fluids from “healthy” or “specially immunized” animals could kill bacteria, so that it was not necessary to resort to cell theory to explain innate and acquired immunity..
The first to experimentally verify the existence of a humoral immune response were Emil von Behring and Shibasaburo Kitasato in the late 1800s. Von Behring and Kitasato demonstrated that the immune responses triggered by diphtheria and tetanus were due to the presence of antibodies against exotoxin.
In the early 1900s, Karl Landsteiner and other researchers realized that other toxins and substances of non-bacterial origin could produce humoral immunity..
The term "antibody" was coined a short time later as a generality, to refer to those specific substances that could function as antitoxins against "antigens".
The word antigen was the term used to define the substances that trigger the production of humoral antibodies.
Effector mechanisms
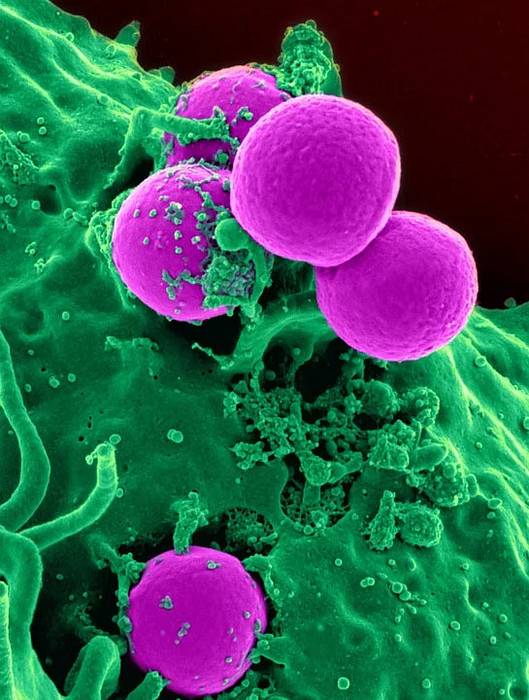
Both humoral immune responses and cellular immune responses are mediated by a type of cells known as lymphocytes..
The main protagonists of cellular immunity are T lymphocytes, while it is B lymphocytes that respond to the presence of foreign antigens and become the antibody-producing cells characteristic of humoral immunity..
Humoral immunity is the main defense mechanism against extracellular microorganisms and other toxins, while cellular immunity contributes to the elimination of intracellular pathogens, which are "inaccessible" to recognition by antibodies..
Phases of the humoral immune response
As well as the cellular immune response, the humoral response can be divided into three phases: one of recognition, another of activation and another of effect..
The recognition phase consists of the binding of antigens to specific membrane receptors on the cell surface of mature B lymphocytes..
Antibodies function as such "receptors" and are capable of recognizing proteins, polysaccharides, lipids and other "foreign" extracellular substances..
The activation phase begins with the proliferation of lymphocytes after the recognition of antigens and continues with differentiation, either in other effector cells capable of eliminating antigens, or in memory cells capable of inducing faster responses after a new exposure to it. antigen.
During the effector phase, the lymphocytes that exert antigen elimination functions are known as “effector cells”, although other cells usually participate, which also participate in the innate immune response, and which phagocytose and eliminate foreign agents..
Lymphocytes and antibodies
The antibodies produced by lymphocytes or B cells have the physiological function of neutralizing and eliminating the antigen that induced their formation and the humoral immune system can respond to a multiplicity of different antigens..
B lymphocytes originate in the bone marrow in response to a defined antigen (they are specific) and this occurs before antigenic stimulation. Expression of specific antibodies triggers proliferation and differentiation responses of more antibody-secreting B cells.
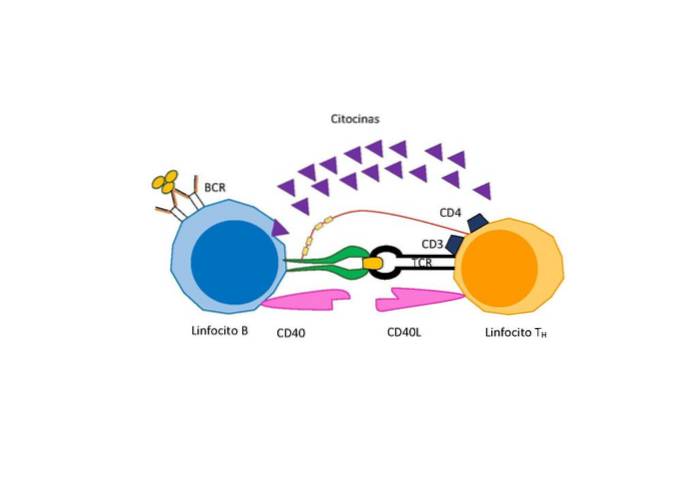
However, depending on the nature of the antigen, an additional signal is needed for differentiation and proliferation that is given by a special type of T lymphocyte called “helper T lymphocyte” that secretes activating factors for B cells..
Immunoglobulins
Since they are mainly found in blood fluids, the antibodies produced by B cells are called immunoglobulins. These protein molecules have two heavy and two light glycoprotein chains linked together through disulfide bridges (S-S)..
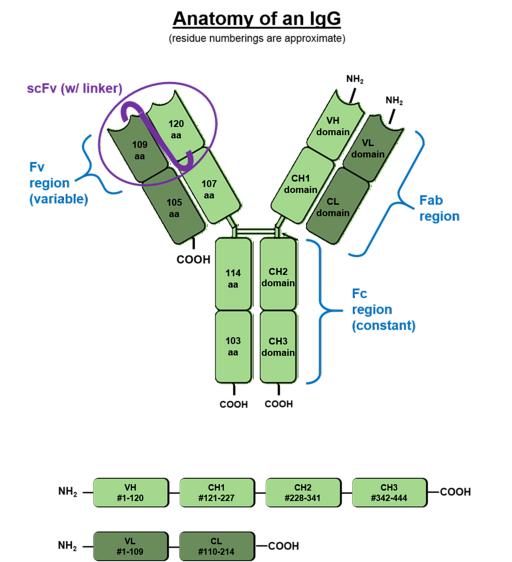
The light chains are known as "kappa" and "lambda", but there are 5 types of heavy chains which have been called gamma (G), mu (M), alpha (A), delta (D) and epsilon (E ).
The combination of light and heavy chains ends with the formation of the immunoglobulins IgG, IgM, IgA, IgD and IgE. The most abundant antibody in mammalian serum in IgG immunoglobulin (approximately 70%).
Each chain of an antibody has an amino terminal and a carboxyl terminal end. The portion capable of binding to antigens is at the amino terminal end, however the carboxyl terminal region is what determines biological activity.
Humoral immune response
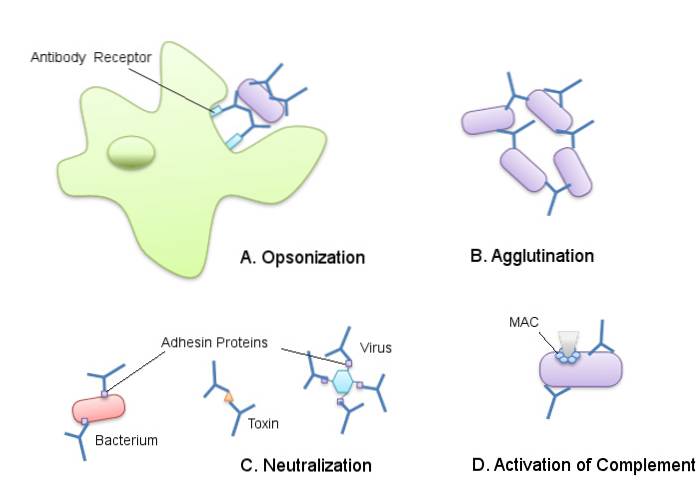
The carboxyl terminal region of IgG antibodies is specifically recognized by phagocytic cells such as neutrophils and macrophages, which have special receptors for it..
This recognition implies contact between the receptor and the antibody and it is this union that facilitates phagocytosis and degradation of antigens inside phagocytic cells..
Unlike IgG, the other classes of immunoglobulins are not found in secretions and tissues. However, they are just as useful in eliciting the immune response..
IgM immunoglobulins (10% of serum immunoglobulins) are potent activators of the complement system, therefore they function in the lysis of antigens and increase resistance.
IgA immunoglobulins (20% of serum immunoglobulins) are produced in lymphoid tissues and are processed and transported to the lung mucosa and gastrointestinal tract. These work to neutralize viruses and other antigens that enter through mucosal surfaces..
IgD is bound to B lymphocytes and functions as an antigen receptor, while IgE (known as the allergic antibody) is bound to the surface of mast cells and basophils through specific receptors. Both immunoglobulins are in very low concentration in serum.
Examples
The antibodies produced by the main effectors of the humoral immune response (B lymphocytes) have the ability to "induce" or "activate" different response mechanisms against different types of threats..
For example, IgG immunoglobulins are activators of what is known as the "complement cascade", which works to neutralize viral particles, thus preventing their binding to host cells..
During pregnancy, the mother transfers antibodies to the fetus through trophoblastic cells of the placenta, which have receptors with high affinity for the carboxyl terminus of immunoglobulins such as IgG.
The humoral response to bacteria that have "capsules" composed of polysaccharides is mediated by immunoglobulin M, which promotes phagocytosis of these microorganisms.
Another important example of humoral immunity is the systemic response to parasites, where IgE "directs" their destruction through eosinophilic cells..
References
- Abbas, A., Lichtman, A., & Pober, J. (1999). Cellular and Molecular Immunology (3rd ed.). Madrid: McGraw-Hill.
- Carroll, M. C., & Isenman, D. E. (2012). Regulation of Humoral Immunity by Complement. Immunity, 37(2), 199-207.
- Kindt, T., Goldsby, R., & Osborne, B. (2007). Kuby's Immunology (6th ed.). México D.F .: McGraw-Hill Interamericana de España.
- Klein, T. (2007). The acquired immune response. In xPharm: The Comprehensive Pharmacology Reference (pp. 1-5).
- Lishner, H., & DiGeorge, A. (1969). Role of the thymus in humoral immunity. The Lancet, two, 1044-1049.
- Medzhitov, R., & Janeway, C. (2000). Innate immunity. The New England Journal of Medicine, 338-344.
- Merlo, L. M. F., & Mandik-Nayak, L. (2013). Adaptive Immunity: B Cells and Antibodies. In Cancer Immunotherapy: Immune Suppression and Tumor Growth: Second Edition (pp. 25-40).
- Silverstein, A. M. (1979). History of Immunology. Cellular versus Humoral Immunity: Determinants and Consequences of an Epic 19th Century Battle. Cellular Immunology, 48(1), 208-221.
- Steinman, R. M. (2008). Linking innate to adaptive immunity through dendritic cells. In Innate Immunity to Pulmonary Infection (pp. 101-113).
- Tan, T. T., & Coussens, L. M. (2007). Humoral immunity, inflammation and cancer. Current Opinion in Immunology, 19(2), 209-216.
- Twigg, H. L. (2005). Humoral immune defense (antibodies): Recent advances. Proceedings of the American Thoracic Society, two(5), 417-421.
- Wherry, E. J., & Masopust, D. (2016). Adaptive Immunity: Neutralizing, Eliminating, and Remembering for the Next Time. In Viral Pathogenesis: From Basics to Systems Biology: Third Edition (pp. 57-69).


Yet No Comments