
Leukopoiesis process, stimulation factors, regulation
The leukopoiesis It is the process of formation and development of leukocytes. It is part of hematopoiesis, the process by which blood cells form, differentiate, develop and mature, including the composition of erythrocytes, platelets and leukocytes.
Hematopoiesis and, therefore, leukopoiesis, are processes that take place in the bone marrow. In the fetus, in addition to the bone marrow, they are also carried out in the liver and spleen.
From birth to about 20 years of age, hematopoiesis occurs in the marrow of all bones. From the age of 20, the marrow of the long bones becomes inactive, with the exception of the upper part of the humerus and the femur. The so-called "red marrow", which is the active bone marrow, is then in charge of hematopoiesis, to differentiate it from the yellow one, which is hematopoietically inactive..
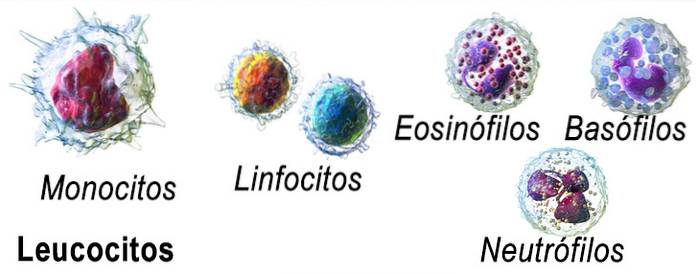
Leukopoiesis includes the differentiation, formation, development, and maturation of various cell lines that give rise to five types of cells:
- Neutrophil polymorphonuclear leukocytes or granulocytes
- Polymorphonuclear Eosinophils
- Basophilic polymorphonuclear cells
- Monocytes
- Some lymphocytes.
Neutrophils are the most abundant leukocytes or white cells in the bloodstream. Despite the fact that there are 500 times more erythrocytes in circulation than leukocytes, 75% of the cells of the bone marrow are of the myeloid series that produce leukocytes.
Article index
- 1 Process (stages)
- 1.1 Myeloid stem cells
- 1.2 Lymphoid stem cells
- 2 Factors that stimulate leukopoiesis
- 3 Regulation of leukopoiesis
- 4 References
Process (stages)
In the bone marrow there are cells called “stem cells” or “stem cells”, stem cells or “hemocytoblasts”. These are progenitor cells for all blood cells from the bone marrow, but they also give rise to osteoclasts, Kupffer cells, mast cells, dendritic cells, and Langerhans cells..
What happens first in the leukopoiesis process is that these progenitor cells divide and give rise to cells called “compromised stem cells”, which are myeloid stem cells and lymphoid stem cells..
Myeloid stem cells
In turn, myeloid cells differentiate and end up producing red blood cells or erythrocytes, platelets, granulocytes or polymorphonuclear cells, and monocytes. Lymphoid cells will give rise to lymphocytes.
For the leukopoiesis process, the development of monocytes and granulocytes is described. So, myeloid cells differentiate into monoblasts and myeloblasts. Monoblasts give rise to "promonocytes", a process in which a change occurs in the shape of the nucleus, which begins to bend. Promonocytes become monocytes. At this stage of development, the nucleus acquires its final horseshoe shape..
Myeloblasts give rise to three cell lines: basophilic promyelocytes, eosinophilic promyelocytes, and neutrophilic promyelocytes. They are cells with cytoplasmic granules that stain with dyes of different pH.
Promyelocytes give rise to myelocytes, thus forming basophilic myelocytes, eosinophilic myelocytes, and neutrophilic myelocytes. In these cells, the nuclei begin to change shape.
Then, the nucleus of these cells takes a "U" shape and "metamyelocytes" or band cells, neutrophilic, basophilic and eosinophilic cells are formed..
Basophilic band cells finish developing by contracting their nucleus to form an “S” -shaped nucleus and become basophils..
Eosinophilic band cells form a bilobed nucleus and give rise to eosinophils and neutrophilic band cells develop a polylobulated nucleus and form neutrophils.
Lymphoid stem cells
Stem cells committed to the lymphoid lineage or lymphoid stem cells give rise to lymphoblasts. These cells, in turn, differentiate and form the so-called "prolymphocytes".
Prolymphocytes continue to develop to give rise to lymphocytes. Two types of lymphocytes are formed in the bone marrow: B lymphocytes and T lymphocytes. B lymphocytes are active cells. They leave the bone marrow into the bloodstream and from there they can go to the lymph nodes. These cells are mature and active cells.
T lymphocytes produced in the bone marrow are immature cells that pass into the blood and reach the thymus or lymph nodes or other lymphoid organs where their maturation or activation process ends..
Factors that stimulate leukopoiesis
The proliferation and differentiation of progenitor cells and of the different stem cells involved until the formation of leukocytes is due to a series of hormonal factors, which act specifically in the different differentiation stages of leukopoiesis.
Interleukins (IL) and colony stimulating factors (CSF) are the main stimulators of stem cell differentiation and subsequent proliferation and maturation of different leukocyte cell lines.
In the presence of interleukin 3 and 5 (IL3 AND 5) and agranulocyte colony stimulating factor (aG-CSF), stem cells differentiate into monoblasts. The formation of myeloblasts depends on the presence of IL3, IL5 and the granulocyte colony stimulating factor (G-CSF).
Interleukin 4 (IL4) participates in the differentiation of myeloblasts along the basophil line. Other factors have been described as the granulocyte and macrophage colony stimulating factor (GM-CSF) and the macrophage colony stimulating factor (M-CSF)..
Some studies show that the absence of some factors, in certain cases, can be replaced by the rest, this implies the joint participation of several factors.
Regulation of leukopoiesis
White blood cells, especially neutrophils, have a very short half-life. Circulating granulocytes have an average half-life of 4 to 8 hours, after which they have to be replaced. Its half-life in tissues is 4 to 5 days.
Monocytes in blood have a half-life of 10 to 20 hours and when they pass into tissues and become macrophages they can last several months. Lymphocytes live for weeks or months and keep circulating between blood and lymph.
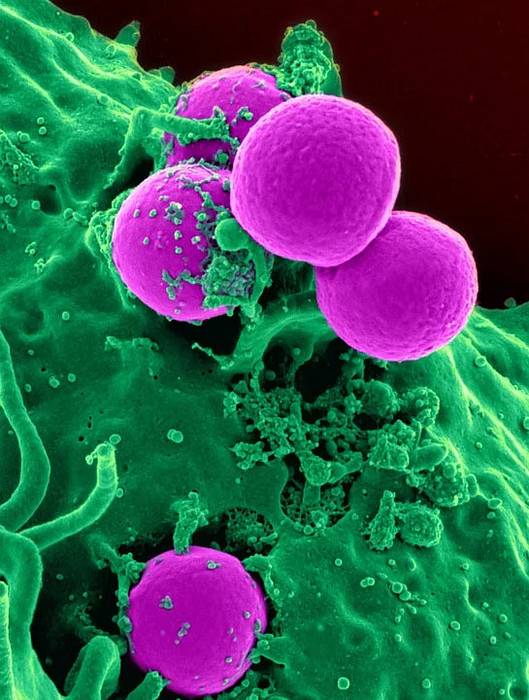
These characteristics require a signal system for replacement and increased production when infections occur that require “extra” amounts of leukocytes. Together, these mechanisms that maintain production and release as needed are what is called the "leukopoiesis regulation process".
The regulation of the differentiation and production of leukocytes depends on a series of substances among which are regulatory factors (growth factors) that are glycoproteins or hormones that stimulate the differentiation of progenitor cells and also keep circulating cells active..
When leukocytes are formed in the bone marrow, not all of them are discharged into the circulatory stream, a part remains in the marrow as a reserve until the circulatory system requires it. The number of granulocytes stored in reserve within the bone marrow triples the number of circulating leukocytes.
These reserves allow the supply for about 5 or 6 days. If an infectious or inflammatory process occurs, macrophages and activated T lymphocytes release factors that stimulate an increase in leukocyte formation, increasing colony-stimulating factors..
Thus, the leukocytosis (increase of leukocytes in the blood) that accompany some infectious processes occur. In mice and probably in humans, the process of regulating the proliferation and renewal of stem cells in the bone marrow involves proteins formed by the gene scl (stem cell leukemia).
References
- Bonilla, Mary Ann; Jakubowski, Ann. Colony-Stimulating Factors in Leukopoiesis. On Humoral Factors in the Regulation of Tissue Growth. Springer, New York, NY, 1993. p. 71-93.
- Ganong, William F. Review of medical physiology. Mcgraw-hill, 2016.
- Guyton, Arthur C .; Hall, John E. Textbook of medical physiology 11th ed. Philadelphia, Perm: Elsevier Saunders, 2006.
- Rebuck, John W .; Bethell, Frank H .; Monto, Raymond W. (ed.). The Leukemias: Etiology, Pathophysiology, and Treatment. Elsevier, 2013.
- Santini, Stefano M., et al. The SCID mouse reaction to human peripheral blood mononuclear leukocyte engraftment. Neutrophil recruitment induced expression of a wide spectrum of murine cytokines and mouse leukopoiesis, including thymic differentiation. Transplantation, 1995, vol. 60, no 11, p. 1306-1314.


Yet No Comments